What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
Infertility can be defined as inability to establish a pregnancy within a specified time, usually one year, in a couple having regular unprotected sexual intercourse. There has been a renewed interest in infertility and reproductive health failure in Subsaharan Africa inspite of its high fertility.
In the African culture, for an infertile couple, the society views infertility as a social stigma with considerable emotional stress. Family and societal pressure on the infertile couple often predispose to marital stress and instability, polygamy, divorce, prostitution and in extreme cases, suicidal tendencies.
The aims of infertility management will include a thorough investigation, treatment of causes, sexuality education and counselling, prognosticate on the chances of success and provide emotional support for the couple.
Definitions
Primary Infertility
Failure to conceive after one year of unprotected cohabitation in a woman who had never conceived previously.
Secondary Inferility
Failure to conceive after a year of unprotected cohabitation in a woman who had previously been pregnant. If the woman had previously breastfed her infant, then exposure to pregnancy should be calculated from the end of the lactational amenorrhoea period.
Pregnancy Wastage
The woman is able to conceive but unable to produce a live-born.
Unproven Fertility/Infertility
This refers to problems sometimes perceived or designated by couples as infertility in demographic surveys, when in fact, the woman is virtually not at risk of conception. The problem may be biological (Lactational amenorrhoea - Anovulation), or among couples practising contraception, or abstinence when the consort is away.
Sterility
This is complete and permanent inability to either impregnate or conceive. Individuals with congenital absence of reproductive organs or who have been sterilized qualify for such a designation.
It is a worldwide problem affecting approximately 10-15% of couples. Global variations have been reported in the incidence of infertility from as low as 1% to 1.5% in Korea and Thialand to as high as 13% - 23% in urban areas of Columbia and rural areas of New Guinea.
The prevalence of infertility is particularly high in Subsaharan Africa, varying from 20-46% in some parts of West Africa. Countries like Gabon, Cameroon, Guinea Equatoria, Central African Republic, Niger, Mali and Zaire have levels of infertility among women aged 25 - 29 years ranging between 7-50%. This high level of infertility suggests that acquired causes of infertility are prevalent in these countries. There are also ethnic and religious bias in the prevalence rates of infertility as seen in these countries.
A WHO multicentre study showed that Africa was the only region where majority of couples had secondary infertility. In developed countries, the level of primary versus secondary infertility was 71% and 29% respectively while comparative figure for Africa was 48% and 52% respectively. Asia, Latin America and East Mediterranean had levels of primary infertility higher than secondary infertility. The same study demonstrates that 64% of females patients in African centres as against 38% of patients in other areas of the world had post-infectious infertility.
In Africa, up to 65% of gynaecological consultations are for infertility. At the University of Ilorin Teaching Hospital, Ilorin, more than 50% of gynaecological consultations are for infertility 6. Post –infectious infertility are relatively commoner in East and Central African countries than the West and South African countries.
It is estimated that by six months of regular unprotected intercourse, 60% of married couples are expected to achieve pregnancy. By 12 months, up to 90% would have achieved pregnancy and at the end of 18-24 months, up to 95% would have achieved pregnancy. Younger women(<18 years) and older women (>35 years) do not have maximal fertility potential like those between the ages of 18-35 years.
The need to investigate will therefore be predicated on the urgent desire to have children by both partners, the age of the female partner especially if she is over 30 years as fertility declines with increasing age after 30 years and if there are certain medical problems that may impair fertility.
Apart from age, marital and ethnic factors highlighted above, other predisposing factors include
- Sociocultural Factors
- Economic Factors
- Psychological Factors
Sociocultural Factors
Cultural practices such as age of marriage, type of marriage (monogamy/polygamy), frequency of intercourse and marriage stability have profound effects on fertility. Dowry, female circumcision, pregnancy care and traditional methods of delivery are plausible variables underlying infertility.
Economic Factors
Micro and macro economic variables have profound effect on fertility potential of the whole population as was witnessed during the severe structural adjustment programmes (SAP) in Nigeria between 1985 and 1995 when the fertility was down to about 5.8 from about 7.0 the previous decade.
Degree of urbanization, education, industrialization and available basic health care facilities are some other indices which affect fertility. War, famine and catastrophes have been shown to reduce fertility rate as shown by the World Wars, Bosnian and Congolese experience.
Certain occupations and labour migration increase the risk to sexually transmitted diseases (STDs) including HIV/AIDS. Lbour migration also separates husband and wife hence reduces exposure of the wife.
Psychological Factors
Emotional tensions have been known to contribute significantly to the functional capability of the hypothalamo-pituitary-ovarian axis, or by causing tubal spasms, vaginismus, dyspareunia, frigidity and decreased male libido. Infertility can thus directly cause emotional stress thus initiating a vicious cycle. Investigations and treatment options in infertile couples could also contribute to their emotional stress.
Counselling and empathy are important prerequisites in assisting infertile couples. The high premium placed on children in African cultures have also contributed, in no small way, to this profound psychological stress associated with infertility.
Post-infectious infertility is commonest in Africa than all other regions of the world. In the developed world, infections play less role while hormonal, congenital and psychological factors are important causative factors.
In general, 10-15% is caused by ovulation disturbances, 30-40% caused by pelvic factors, 30-40% is associated with abnormalities in the males, and 10-15% associated with abnormalities in the cervix. In about 10% of couples, with the current techniques of investigations, it is impossible to diagnose the cause of infertility, hence unexplained infertility.
Female Infertility
- Tubal Factor
- Ovulation Factor
- Uterine Factors
- Cervical Factors
- Vaginal Factors
Tubal Factor
- The tubal factor is the commonest cause of infertility in the female. Tubal abnormalities, present in 50-70% of infertile women, are due to previous pelvic inflammatory disease. The sequale of such inflammatory process is chronic PID, tubal blockage, hydrosalpinges and peri-adnexal adhesions.
- The PID is usually caused by STDs with N.gonorrhoea, C. trachomatis and T. mycoplasma (Ureaplasma Urealyticum) being the common pathogens. Postpartum and postabortal infections are also important causes of PID.
- Less common causes include infection of IUDs, post surgical conditions (appendicitis, diverticulitis), tuberculosis, schistosomiasis and pelvic surgery.
- Endometriosis is a rarer cause of tubal obstruction in our environment.
- Psychosomatic factors has been implicated in tubal dysfunction while congenital tubal aplasia or presence of convoluted tubes are extremely rare causes of female tubal infertility.
Ovulation Factor
- 10-15% of female infertility is caused by anovulation and luteal phase defficiency in this environment.
- Polycystic ovarian disease (Stein-Leventhal Syndrome) is characterized by enlarged ovaries with multiple follicular cysts, menstrual irregularities, hirsutism, obesity and some insulin resistance.
- Other anovulatory causes include
- hypothalamic dysfunction of environmental, physical or emotional origin pituitary adenomas with or without hyperprolactinomas and
- hypogonadism with or without luteal phase deficiency.
- Rarer causes include pituitary hypofunction (sheean’s syndrome), primary ovarian failure e.g Turner’s syndrome, ovarian resistant syndrome and contraceptives (oral, injectables and norplant).
- An uncommon cause of anovulation is luteinised unruptured follicle syndrome in which there is failure of ovulation due to intrinsic defect in the epithelial surface of the ovary to permit ovulation.
- Hormone production and endometrial luteal phase development are satisfactory but there is failure of ovulation.
Uterine Factors
- Common uterine factors such as uterine fibroids and uterine polyps are often associated with infertility or reproductive wastage. They cause distortion of the uterus and fallopian tubes leading to infertility.
- Postpartum, post-abortal, post-surgical or post-tuberculous endometritis may cause intrauterine adhesions (uterine synechiae).
- Insufficient decidual layer formation with lack of or improper implantation may result from luteal phase defficiency.
Cervical Factors
- Cervical factors resulting in infertility include hormonal imbalance which causes poor quality cervical mucus impenetrable to the sperm, cervical infections with sperm antibodies, cervical stenosis due to congenital defect or previous cervical surgery (cauterization or cone biopsy).
- The role of immunological factors in cervical infertility in which women develop antisperm antibodies has received considerable attention in the last two decades as a common cause of hitherto unexplained infertility.
Vaginal Factors
- Congenital or developmental defects such as transverse or longitudinal septa, imperforate hymen or stenosed fourchette can contribute to infertility.
- Severe vaginitis causing dyspareunia or vaginal stenosis following chemical vaginitis are known though rare causes of infertility.
Male Infertility
- Interest in male infertility, responsible for 30-40% of infertile couples, has increased over the years.
- Subacute or chronic infection of the male genital tract is a common cause of poor sperm production or function.
- Common organisms implicated include
- Bacteria (gonococcal, coliform, staphylococcal),
- Viral (mumps orchitis, infectious mononucleosis),
- Parasitic (schistosomiasis, toxoplasmosis).
- Vasal or epididymal blockage may result from these infections.
- Congenital (cryptoorchidism), acquired (varicocele, trauma, torsion of the testis) and certain endocrine disorders such as diabetes mellitus, hyperprolactinaemia, hypogonadism can reduce sperm production and function.
- Chromosomal abnormalities (47XXY/46XX) can cause disorders in sperm production and function. Addictive behaviours such as alcoholism and heavy smoking play a part in lowering sperm function in men.
- Environmental factors (heavy metals, excessive heat, radioactivity) and chronic stress can reduce sperm function.
- Varicocele can be unilateral or bilateral and are present in approximately 15% postpubertal males and 20-40% of infertile males.
To the average medical practitioner in Africa, it is usual to see the woman present first for infertility. It is a cultural belief that the is to blame for the infertility in the couple. Though it is preferable to see both partners at the first visit, often this is not practicable hence it is reasonable to commence with the clinical evaluation of the wife. Usually, through a combination of tact, patience and proper counselling, it is not too difficult to elicit the support and presence of the male partner.
A detailed history should be methodological and complete taking special note of duration and severity of the problem, sexual history, history of previous treatments (orthodox and traditional), history of previous abdominal and pelvic infections, history of abdominal and pelvic surgeries (including pregnancy termination). Complete obstetric history should be taken while type of profession and or occupation of both partners, socioeconomic conditions, cultural and religious background of the couple should be clarified e.g Oligo-asthenospermia is relatively frequent in long distance professional drivers.
Polygamy/polygny is common in African societies especially among muslims while workers on shift duties may find it difficult to also meet up with a ‘timed’ intercourse.
A detailed history of past medical history could unearth antecedent or coincidental medical conditions such as diabetes mellitus, hypothyroidism, chronic granulomatous diseases etc which may impair fertility.
A complete and detailed physical examination of the couple is essential.
History
CLINICAL FEATURES IN AN INFERTILE COUPLE .
Male
- Duration of infertility
- Profession/Occupation
- Previous history of Sexually Transmitted Diseases, Mumps orchitis
- History of congenital malformations
- Previous history of abdominal / genital surgery including herniorrhaphy and hydrocelectomy.
- History of diabetes mellitus and other endocrine disorders.
- Alcoholism, Excessive smoking
- History of chronic drug use – Brinerdin, Aldomet, Thiazides and Anticonvulsants.
Female
- Duration and severity of infertility
- Detailed previous obstetric history
- Profession/Occupation e.g Students, Commercial sex workers, Young professionals
- Gynaecologoical history including menarche, ketamenia, dysmenorrhoea, menstrual flow pattern etc.
- Previous history of sexually transmitted diseases, mumps in childhood, congenital malformation.
- Previous history of abdominal and pelvic surgery (including pregnancy termination, myomectomy etc).
- Previous history of contraception.
- Previous history of tuberculosis.
- Endocrine disorders.
- Alcoholism, Excessive smoking and chronic drug use.
Physicalexamination
Female
- Nutritional status – Height, Weight, Anaemia etc
- Endocrine diseases – Thyroid, Diabetes mellitus.
- Breasts – galactorrhoea, poorly developed breasts as in Turner,s syndrome.
- Hirsuitism, Voice changes
- Abdominal surgical scars – appendicectomy, laparascopy and laparotomy for intra-abdominal lesions.
- Previous cesarean section scars.
- Pelvic examination- congenital malformation of genital tract, PID, Endometriosis, Adnexal pathologies.
Male
- Habitus, General physical examination.
- Genitalis –
- Penis – size, hypospadias, epispadias.
- Urethral stricture
- Testis - size, location and position, consistency, varicocele and other tumours.
- Prostate - size, consistency, milking of the prostate.
Investigations
Ideally, the couple need to be investigated together. Since it is known that in African settings, in 30 – 40% of infertile couples, both husband and wife have discernible problems. Proper counselling on the need for these investigations should be offered.
Efforts should be made not to over or under prognosticate the chances of the couple. Where it may not be possible to start with the couple together, the woman can start her own investigations pending the time the husband could be invited and investigated.
Investigation of the infertile couple should start with general investigations such as haemogrammes (including ESR), urethral, cervical or high vaginal swab, urinalysis, urine culture and sensitivity.
- Semen analysis
- Hormonal evaluation
- Special sperm function tests
- Tests of ovulation
- Tests of tubal patency
Semen Analysis
Semen analysis is the specific investigation for male infertility and should be done early. It should be stressed that 2-3 tests should be done at least 1 month interval before a conclusion could be reached as to the normality of the test especially if a subnormal result was obtained.
The semen sample is normally obtained after 3-5 days of abstention. The sample obtained by masturbation is better for analysis than that obtained by withdrawal method or with the aid of condoms as these contain spermicides.
The sample is collected in a sterile wide mouthed container and should be sent to the laboratory within 2 hours. Parameters such as volume, colour, pH value, consistency, spermatozoal count per ml, motility and morphology of spermatozoa and fructose contents are examined.
The sperm sample could also be cultured for microorganisms when indicated and the sensitivity pattern to antimicrobials shown.
The computer-assisted semen analysis (CASA) systems couple video technology and sophisticated microcomputers for automatic image digitalization and processing. This technology was developed for more objective assessment of seminal parameters over the subjective measurements of standard semen analysis. CASA permits the measurements of additional motility parameters such as curvilinear velocity, straight line velocity, linear and flagellar beat frequency.
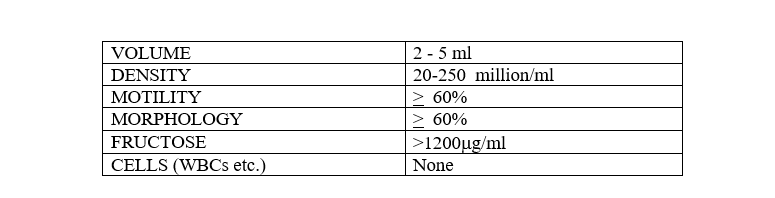
Semen with volumes <1ml or >6mls per ejaculate, density <15 million/ml or >250 million/ml, poor motility and morphology may be incompatible with normal fertility.
Hormonal Evaluation
- Routine evaluation of hormonal parameter is not necessary unless sperm density is extremely low or there is clinical suspicion of an endocrinopathy.
- The incidence of primary endocrine defects in infertile men is less than 30%. Such defects are rare in men with a sperm concentration of >5 million/ml.
- When an endocrinopathy is discovered, specific hormonal therapy is often successful. Follicle Stimulating Hormone(FSH), Luteinizing Hormone(LH), Testosterone and Prolactin levels are checked to differentiate hyper or hypogonadism, primary and secondary testicular failure as well as obstructive lesions.
- In men with a history of precocious puberty, one should consider Congenital adrenal hyperplasia (CAH), hence serum levels of 17-OH progesterone are evaluated. Other pituitary hormones like ACTH, TSH and GH could be assessed but this is rarely necessary.
Chromosomal studies
- Chromosomal studies may be specially indicated in men with small testes, azoospermia and elevated FSH levels to look for both autosomal and sex chromosomal abnormalities.
Antisperm antibodies
- Antisperm antibodies, though not an absolute cause of infertility, may reduce the likelihood of pregnancy.
- These antibodies may impair sperm function by attaching to the plasma membrane of the spermatozoa, encouraging sperm agglutination particularly in the presence of infections. Antisperm antibodies should be suspected in couples who persistently have abnormal post-coital tests. Immunological factor may be responsible for up to 20% of unexplained infertility.
Special Sperm Function Tests
- Sperm-cervical mucus interaction (post-coital test, PCT)
- This test assesses the ability of sperm to penetrate and progress through the cervical mucus. Cervical mucus is examined 2-8 hours after intercourse at the time of expected ovulation.
- The presence of greater than 10-20 motile sperms per high power field is generally accepted as a normal PCT.
- PCT is a bioassay that provides information concerning sexual function, sperm motility and sperm-mucus interaction. A positive result implies normal semen and mucus.
- A poor result in an individual with normal semen parameters implies either cervical abnormalities or the presence of sperm antibodies.
- Sperm Penetration Assays.
- Penetration of an oocyte requires sperm capacitation, acrosome reaction, fusion and incorporation into the oocyte. Cross-species fertilization is normally prevented by the zona pellucida.
- Hamster eggs stripped of the zona pellucida can be penetrated by human sperm. This in-vitro functional test measures the penetration ability of the sperm.
- The end point of this assay is penetration of the ovum and decondensation of sperm heads. The percentage of oocytes penetrated and the number of sperm penetrating each oocyte are measured. Sperm that are capable of multiple penetrations per oocyte appear to have greater fertilizing potential than sperm that do not penetrate.
- The result of the sperm penetration assay (SPA) have primarily been used to predict the results of assisted reproductive technique, in particular, in-vitro fertilization.
- Men with sperm of low SPA score are less likely to achieve a spontaneous pregnancy than those with a high SPA score. However, abnormal penetration does not indicate that fertilization cannot occur, nor does good penetration assure fertilization.
- Generally speaking, less than 10% penetration is evidence of sperm dysfunction and male infertility. Although the SPA is a reliable indicator of the fertilizing capacity of human spermatozoa, it does not predict the ability of sperm to bind to and penetrate zona pellucida or the sperm’s motility and progression in the female reproductive tract.
Tests Of Ovulation
The regularity of a menstrual cycle does not confirm occurrence of ovulation, though most women who have regular cycles tended to ovulate regularly.
Tests of ovulation are numerous including
- Basal Body Temperature(BBT),
- Endometrial biopsy,
- Hormonal Assay,
- Serial ultrasound folliculography,
- Cervical mucus and vaginal cytological changes.
However, the only confirmatory evidence of ovulation is pregnancy or observation of the corpus luteum during laparascopy.
- Basal Body Temperature.
- In this environment, BBT is usually reserved for literate and well motivated patients.
- Temperatures should be taken at the same time each day and by the same route, preferably just after rising from sleep each morning taken either by axillary method or oral route.
- A BBT chart is kept on daily basis and a biphasic pattern suggests that ovulation had occurred.
- In ovulatory cycles, the elevated temperatures post-ovulatory is brought about by the thermogenic effect of progesterone as opposed to monophasic temperature pattern in anovulatory cycles.
- Endometrial Biopsy.
- Endometrial biopsy is commonly used to determine the occurrence of ovulation.
- A histological examination of an endometrial sampling on day 21 or 23 of the menstrual cycle will show secretory endometrium in ovulatory cycles compatible with the day of endometrial sampling while simple hyperplasia or atrophic changes will be seen in anovulation.
- An added advantage of this method is that it also permits the diagnosis of tuberculous endometritis and luteal phase deficiency. Inadequate or improper endometrial sampling could lead to errors in reporting.
- Hormone Assays.
- Serum progesterone assay using radioimmunoassay technique measures progesterone levels on day 21 or a progesterone index (mean value of days 20,21,22 samples).
- There is inter-laboratory variations but values less than 10 mmols/l are unsatisfactory. Low levels (< 5mmols/l) will suggest anovulation while values between 5-10mmols/l may suggest luteal phase defect.
- Serial Ultrasound Folliculography
- This has now been made easier with the use of sector scanner and a vaginal probe.
- Serially, the ovaries are scanned from the beginning of the menstrual cycle when the follicles measure on an average 3-5mm to the peri-ovulatory period where diameters of up to 20-23mm could be obtained.
- Usually a dominant follicular diameter of >16mm is highly suggestive that ovulation will occur.
- Following ovulation, the follicular diameter will diminish due to the discharge of its contents and eventual transformation into a corpus luteum.
- Serial ultrasound folliculography is extremely useful in monitoring ovulation during induction of ovulation and assisted reproductive techniques.
- Cervical mucus and vaginal cytological changes
- They are not routinely used in clinical practice in our environment.
- However, a semi-quantitative estimation of four parameters – the amount of cervical mucus, spinnbarkeit (threadability), crystallization capacity of the mucus and the degree of opening of the external os corresponds well with the hormonal interplay during the index menstrual cycle.
- Each of the parameters may receive a score of 0-3 points with the total score being 0-12 points.
- Since the amount and type of mucus produced by the endocervical mucosa are under hormonal control, the cervical score is an indirect indicator of relative levels of estrogen and progesterone.
- Estrogen stimulation results in a high score while progesterone results in a low cervical score.
- A low cervical score indicates either lack of estrogen or a high progesterone level and a high score (>8 points) indicates distinct estrogen stimulation unopposed by progesterone action.
- During a normal ovulatory cycle, the cervical score is low at the beginning, becomes positive 5-7 days before the temperature nadir, increases steadily during the pre-ovulatory period reaching a high plateau within 2-3 days of ovulation, declines 1-3 days following the temperature nadir, and becomes negative 5 days after ovulation.
- Vaginal cytology can also be used to monitor ovulation period. Local inflammation, douching and insertion of foreign bodies can alter the results obtained.
- The presence of multilayered navicular cells with interstitial oedema in the vaginal cytology smear may suggest progesterone dominance following ovulation.
Tests Of Tubal Patency
Several tubal patency tests exist involving insufflation with air, water or carbondioxide. These are simple, cheap and easy to perform but it has been shown that these methods are grossly inadequate, and the WHO recommend that they should be abandoned even as a screening procedure.
Laparascopy plus dye hydrotubation is regarded as the ‘gold standard’ for the assessment of tubal patency. Moreover, this procedure may disclose other unsuspected infertility factors such as endometriosis and pelvic adhesions. However, laparascopy requires hospital admission, anaesthesia and a fully equipped operating room.
Hysterosalpingography (HSG), conversely, remains a safe and simple procedure that outlines the lumen of the uterine cavity and the fallopian tubes. HSG and laparascopy are found to be similar in 80% of cases with a similar number of false positives and false negatives. HSG thus remains the best screening test in our environment. The ideal technique, however, requires a television fluoroscopy monitor which is not readily available in many third world countries. A simplification of the technique was found in a plain X-ray of the pelvis taken 15 minutes after the injection of contrast material and this has been shown to have a good correlation with the findings of a complete HSG.
note
Timing of Investigations
This is necessary in order to reduce time wastage in the investigation and treatment of the infertile couple. It is recommended that these tests could be completed within a single month of a menstrual cycle and the results provided to guide treatment during the next menstrual cycle.
Following the initial assessment of the couple in the day preceding the onset of menses, a semen analysis could be ordered. BBT can be started on the first day of her menses while Hysterosalpingogram (HSG) can be done between days 7-11 and a PCT on day 14.
Laparascopy dye test, endometrial biopsy and hormone assays could be performed on day 21. The results of these tests would now form the template upon which further assessment and treatment would be based.
Treatment Of Infertility
Following a detailed investigation, the treatment offered can be by conventional methods or by newer assisted reproductive techniques.
Sufficient counselling should be given to the couple explaining in detail the results of the investigations, implications on treatment modalities and possible prognosis without unduly raising the expectations of the couple.
A modest guarantee of pregnancy should be given because even when we correct all known causes of infertility the actual process of conception still depends on the biological fecundity of the couple and the frequency with which they have sexual intercourse.
Treatment Of Male Infertility.
- Effective treatment for the infertile or subfertile male is divisible into three categories – surgical, medical and others.
- Surgical treatment aims to correct specific physical defects in order to improve sperm quality. Surgical ligation or transvenous embolization has been used to improve semen parameters in selected cases of varicocele.
- Blockage of the vas deferens or epididymis should be corrected by microsurgical techniques which has considerable improved pregnancy rates within the last decade. Pregnancy rates following microsurgical vasovasostomy and vasoepididymostomy range between 40-70%.
- Congenital absence of vas or scarring of the vas deferens/epididymis though not amenable to standard surgical correction, is best handled by directly aspirating sperm from the epididymal tube to be used in Zygote Intrafallopian Tube Transfer (ZIFT).
- Infertile men with hyperprolactinaemia and prolactinomas respond well to bromocryptine while gonadotrophin are useful in hypogonadotrophic hypogonadism.
- Spermatogenesis may also be improved by medical or surgical treatment of hyperthyroidism, hypothyroidism, cushing’s disease, diabetes mellitus etc.
Other Treatment Modalities
- Artificial Insemination
- Assisted Reproductive Techniques(Art)
- InVitro Fertilization+Embryo Transfer (IVF+ET),
- Gamete IntraFallopian Transfer(GIFT),
- Zygote IntraFollicular Transfer(ZIFT) and
- Intracytoplasmic Sperm Injection(ICSI).
Artificial insemination may be performed with either the husband’s sperm (AIH) or donor sperm (AID). Homologous artificial insemination is usually reserved for specific indications such as male impotence, severe hypospadias, retrograde ejaculation or abnormal semen parameters.
A variation of artificial insemination with the husband or donor semen is intrauterine insemination indicated in cases of cervical factors that are not amenable to conventional treatment methods, abnormal PCT of undetermined nature and certain sperm defects.
It is preferred now to use frozen semen (stored for at least 6 months) rather than fresh semen for AID in view of the risk to HIV infection.
Haemoglobinopathy, chlamydia infection etc should be excluded in the donor.
Insemination is usually performed as close as possible to the time of ovulation. In intrauterine insemination, up to 0.3-0.5mls is slowly injected through the intracervical catheter, the rest is sprayed over the cervical mucus or placed in a cervical cap which may be left in place for few hours.
Artificial Insemination Homologous(AIH) has reported pregnancy rate of 20-50% while for AID, the value is between 40-50% within six months of donor insemination. In order to enhance fertility and improve pregnancy rates in couples with unexplained infertility, superovulation with clomiphene citrate or human menopausal gonadotrophin (HMG) can be combined with intrauterine insemination.
These techniques can be used to treat both male and female infertility when other forms of treatment has failed and AID is unacceptable to the couple.
Asthenospermia and morphologic abnormalities hitherto contraindications to ART have been shown to be capable of being used for fertilization successfully in ART.
Techiques that have been used in male infertility included
Couples requesting IVF for male infertility should be clearly counselled concerning their modest but diminished chances of successful pregnancy but need not be denied an IVF because of poor PCT result
Treatment of Female Infertility
Tubo-Peritoneal Factor
Tubal infertility is the commonest cause of secondary infertility in women. When tubes are occluded, macro or microsurgical repair of the tubes are carried out.
The various restorative tubal surgeries include salpingolysis, cuff salpingostomy, cornual anastomosis(for proximal tubal disease), excision and end to end anastomosis and tubal implantation into the uterus.
Despite the 80-90% tubal patency rate obtained in many centres, pregnancy rates have generally varied between 15-50% due to a variety of factors amongst which are
- Most tubal diseases seen in Africa are in advanced stages with significant pelvic adhesions
- Limited expertise and equipments to do microtubal surgery
- Significant post-operative adhesions from the macrosurgical technique and
- A patent tube does not necessarily guarantee a functional tube. It is expected that with improvements in surgical techniques (especially microtubal surgical techniques), early tubal diseases at presentation, prevention of post-operative infection (including STDs) and better patient selection, improved results could be obtained.
Peritoneal factors such as pelvic adhesions arising from STDs, Pelvic Inflammatory Diseases(PID), endometriosis, ruptured viscera etc are best treated with adhesiolysis.
The best results are obtained in those with mild pelvic adhesions while moderate-severe pelvic adhesions may infact worsen the prognosis for the woman.
The use of ventrosuspension in pelvic surgery for infertility is recommended to reduce postoperative posterior pelvic adhesions. Endometriosis are best handled with a combination of Danazol and adhesiolysis.
Endocrinopathy
In patients with anovulatory disorders, ovulation could be induced with either Clomiphene citrate (Clomid) tabs or Human gonadotrophin (HCG) injections.
It is necessary to initiate Clomid therapy from the 50mg daily scheduled to a maximum of 200-250mg twice daily regimen. If after 6th treatment cycles, the patient does not ovulate, the chances are that the patient may not.
It is also important to avoid hyperstimulation syndrome in such women. The success rate with Clomid therapy in suitable cases have been estimated to be between 80-85% 6.
In amenorrhoiec women with normal genital apparatus, menstruation can be recalled following a PCT followed by Clomid and HCG therapy.
Hypergonadotrophic hypogonadism associated with hyperprolactinaemia is treated with bromocryptine to restore normal cycles and ovulation.
Assisted Reproductive Techniques
These procedures are used for infertile couples who cannot get pregnant through conventional means. Much interest has been generated by these procedures since the first success was recorded in 1978 by Edwards and Steptoe with the birth of Loius Brown through IVF + ET. Since then, other procedures have been introduced namely-GIFT, ZIFT, Pronuclear Stage Tubal Transfer (PROST), ICSI etc .
These procedures are now a part of the procedures to manage intractable infertility in many developed countries. The specific indications for the procedures include irreversible tubal infertility, severe oligospermia and unexplained infertility.
At present the success rate for IVF+ET and GIFT in developed countries varies from 20-35% per treatment cycle. However, experience from developing countries including Nigeria has not been encouraging where results have been poorer.
Some of the factors responsible for this included
- High cost of the procedures,
- High cost of setting up and maintaining these centres,
- Skilled expertise may not be readily available and
- Basic infrastructural facilities which complement the attainment of success in these procedures are lacking.
Also, in developing countries, these procedures are not cost-effective, compete with basic health care necessity and if though they are potentially useful for up to 10-15% of infertile couples, considerably few number are able to utilise these for the above-mentioned reasons.
Other Treatment Modalities
Adoption
- Adoption is considered an option for those couples who have tried without success in infertility management.
- In African societies, like in many other traditional societies, adoption is still considered unacceptable and almost a taboo in some societies.
- In adoption, adequate legal backing, social welfare programmes, proper monitoring needs to be put in place in order to protect the interest of the adoptee, adopter and the society at large.
Surrogate Motherhood
- This is a situation in which an infertile woman procures the services of a fertile woman to carry a pregnancy for her using the infertile woman husband’s sperm for fertilization. Such infertile women invariably must have had many unsuccessful attempts at infertility management (both conventional and ART).
- The surrogate mother is therefore expected to carry the pregnancy and following childbirth, hands over the newborn to the infertile woman - in other words her uterus was hired for a service.
- This obviously requires considerably legal procedures, psychological counselling and perhaps adequate financial compensation to prevent the problems of regrets by the surrogate mother.
- In extreme cases, the surrogate mother may resort to murder of the infertile couple and the baby.
Cloning
- This is a controversial option that may be open to an infertile woman in her desperation to have an offspring.
- It is still considered to be at experimental stage inspite of the birth of Dolly-sheep. It is expensive and still illegal in most parts of the world to carry out research on human cloning because of ethical, technical, socio-cultural and religious objections to this procedures.
- It is however interesting to note that cloned animals have been shown to age faster, have more congenital defects and have more auto-immune disorders.
Most of the causes of infertility, particularly secondary infertility, are preventable. In Africa, 80-85% of infertile couples have post-infective causes.
Measures aimed at preventing pelvic infections in Africa include
- Reduction in incidence of stds and pids
- Prevention of intrapartum and postpartum infections
- Prevention of post-abortal sepsis.
Other measures suggested include a more proactive abortion law for the country, increased use of contraceptive to reduce or prevent unwanted pregnancies, improvement in the women’s status, equality of right to education, work and reproductive health decisions and affordable, accessible and functional antenatal care services including skilled delivery.
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions