What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
Definition
Artificial initiation of labor after fetal viability (28 weeks gestation) before its natural onset with the aim of achieving vaginal delivery at minimal risk to the mother and the baby.
An intervention designed to artificially initiate uterine contractions leading to progressive dilatation and effacement (thinning and shortness of ther cervix) and delivery of the baby.
Includes both women with intact membrane and spontaneous rupture of membranes but who are not in labor.
In contrast, augmentation of labor is an intervention for increasing the rate of progress of labor after its onset. Stimulation when the membrane has ruptured spontaneously.
Aim of induction
To achieve vaginal delivery with minimal risk to the mother and the baby
Failed induction of labour is the inability to achieve vaginal delivery following induction of labour irrespective of the reason for the failure.
It is not a complete diagnosis if the cause is not stated e.g. failed induction of labor due to cord prolapse, CPD, fetal distress, etc.
Incidence varies widely from 3-20%
Depend on the facilities for diagnosing antenatal problems in pregnancy and monitoring.
Maternal
Preeclampsia, eclampsia- not an indication for cesarean section so labor can be induced.
Previous precipitate labor- lasts about 4 hours from its beginning to the end.
SPROM
Post term pregnancy
Previous unexplained IUFD- for example, if a previous fetus died at 40 weeks without any identified reason, labor can be induced before 40 weeks to prevent recurrence.
Medical conditions-DM, Heart, renal disease, hypertension
Social reasons such as a woman requesting to be delivered before term for example, for example, so that the child’s birthday coincide with that of the father is not an indication for induction.
Fetal
IUFD
Fetal anomaly incompatible with life
Severe IUGR
Rh isoimmunisation
Failure leading to Caesarean delivery
Uterine hyperstimulation
Fetal distress/ death
Rupture uterus
Intrauterine infection, sepsis
Iatrogenic delivery of preterm infant
Precipitate/dysfunctional labor
Increased risk of operative vaginal delivery
Increased risk of birth trauma
Increased risk of PPH- every woman to be induced should have prophylaxis for PPH
Maternal
More successful treatment or improvement of medical condition caused or aggravated by pregnancy such as hypertensive disorders, sickle cell disease, diabetes mellitus.
Relieving emotional distress after fetal death in utero.
Alleviating anxiety about the fetal well-being especially in the presence of risk factors.
Relieving maternal discomfort e.g. in polyhydramnios.
Allowing essential treatment to be commenced e.g. radiotherapy for malignancies.
Fetus
Reduces the risk of IUFD
It might help improve growth and development of fetus outside the uterus in IUGR.
- A satisfactory indication and competence.
- Assess fetal maturity/confirmation of GA (ensure age of viability is attained).
- Adequate pelvis.
- Exclude contraindications to vaginal delivery.
- Patient counseling and consent.
- Facility for EMCS or instrumental delivery in case induction fails.
- Favorable cervical status – using Bishop Score, BScore of at least 6. Bishop score 6 or higher predicts successful induction and vaginal delivery, if not at or greater than 6, then cervical ripening indicated for achieving dilation.
- Access to blood (grouped and cross matched or grouped and saved) should there be need for it.
note
Why is cervical ripening important?
- It has been shown that the nearness to spontaneous labor by the cervix before induction, the better the outcome.
- Cervical status is accessed using the Bishop score. A favorable score is a score of 6 or more. A score that is less than 6 is unfavorable and cervical ripening will be needed to increase the chance of a successful induction.
The Bishop Score
Bishop produced a scoring system to quantify cervical status and how far this process had progressed prior to the Induction of labor.
High scores (a ‘favorable’ cervix) are associated with an easier, shorter induction that is less likely to fail.
Low scores (an ‘unfavorable’ cervix) point to a longer IOL that is more likely to fail and result in Caesarean section.
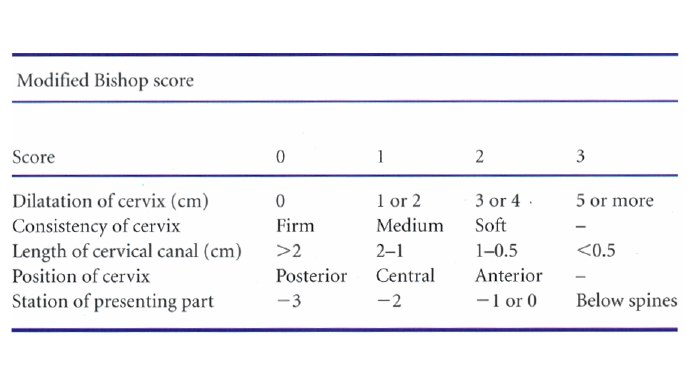
There are 5 parameters. The maximum score for two of the parameters is 2 and the maximum score for the remaining three parameters is 3 giving a possible total score of 13.
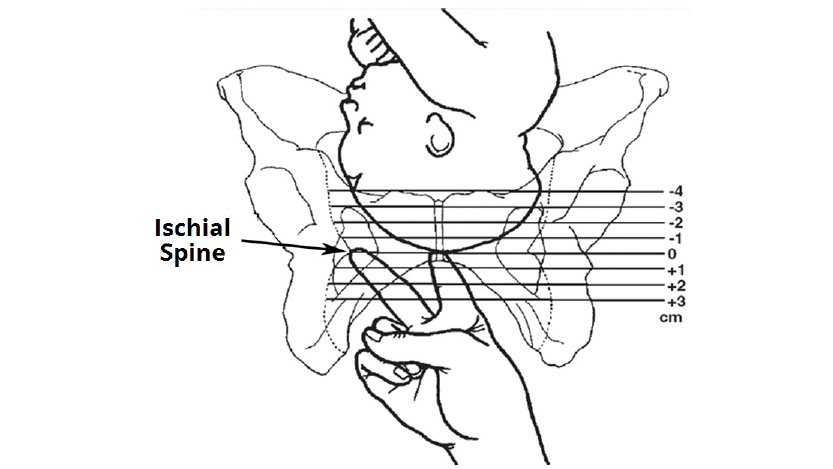
Four of the parameters are about the cervix and one is the station of the presenting part. The station is the relationship of the presenting part to the ischial spines. It indicates how far the presenting part has descended into the mother’s pelvis.
Some methods can ripen the cervix only and there are some that can both ripen the cervix and induce labor.
Cervical ripening only:
- Osmotic dilators e.g. dilapan or lamineria tent
Induction only:
- Oxytocin
Cervical ripening and induction of labor:
- Prostaglandins E2, E1
- Cervical Foley catheter- quite effective for cervical ripening but not as effective for induction.
It can also be surgical, mechanical, or hormonal.
Surgical:
- Amniotomy with oxytocin infusion
Mechanical (cervical ripening):
- Balloon catheters
Hormonal (induction):
- Oxytocin
- Prostaglandins- PGE2, misoprostol
- Relaxin
- Nitric oxide donors
- Mifepristone
Mechanical methods
Hygroscopic dilators
They absorb endocervical and local tissue fluids, causing the device to expand within the endocervix and provide mechanical pressure. These dilators are either natural osmotic dilators (e.g., Laminaria japonicum) or synthetic osmotic dilators (e.g., Lamicel).
Advantages:
- Outpatient placement
- No need for fetal monitoring
Risks:
- Fetal and/or maternal infection
Synthetic dilators:
- These work like the laminaria.
- Examples are
- Lamicel (polyvinyl alcohol polymer sponge impregnated with 450 mg of magnesium sulfate).
- Dilapan (made from a stable non-toxic hydrophilic polymer of polyacrylonitrite).
- These dilators are cheap and easy to use.
- They may be suited for patients with previous uterine scars in whom pharmacological means of induction are contraindicated.
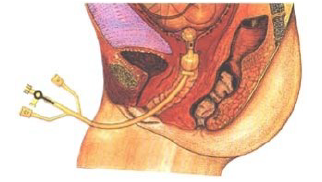
Placement of intracervical catheter balloon
A fluid filled balloon is inserted inside the cervix. The Balloon provide mechanical pressure directly on the cervix which respond by ripening and dilation. A Foley catheter (26 Fr) or specifically designed balloon devices can be used.
Technique of balloon placement:
After sterilization and draping, the catheter is introduced into the endocervix either by direct visualization or blindly by sliding it over fingers through the endocervix into the potential space between the amniotic membrane & the lower uterine segment.
The balloon is inflated with 30 to 50 ml of normal saline and is retracted so that it rests on the internal Os.
Catheter is removed at the time of rupture of membranes or may be expelled spontaneously which indicate a cervical dilatation of 3-4 cm.
If catheter does not fall off after 12-24hours, it can be deflated, removed and repassed after 12 hours
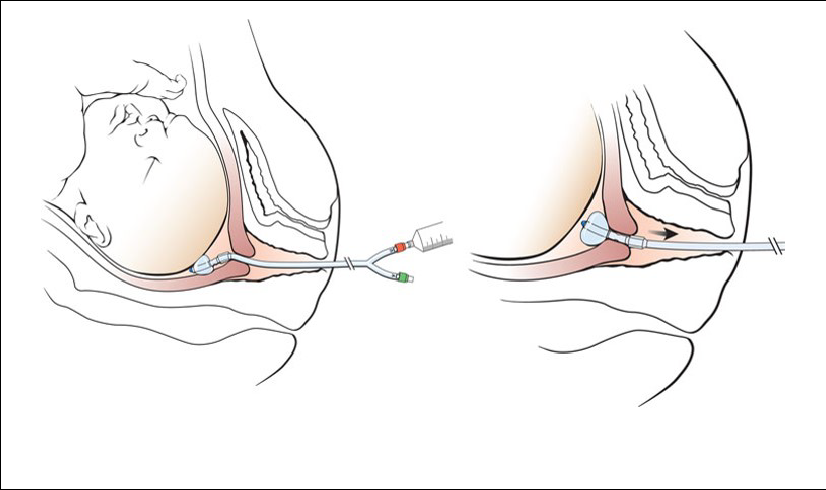
The Atad Ripener Device in place with the two balloons inflated. The uterine balloon is at the internal os and the cervicovaginal balloon is at the external Os.
Stripping the membranes
Stripping the membranes mechanically dilates the cervix which releases prostaglandins. The membranes are stripped by inserting the examining finger through the internal os & moving it in a circular direction to detach the inferior pole of the membranes from the lower uterine segment.
Risks include patient’s discomfort, infection, bleeding from undiagnosed placenta previa or low lying placenta, and accidental ROM.
The Cochrane reviewers concluded that stripping the membranes, when used as an adjunct, decreases the mean dose of oxytocin needed and increases the rate of normal vaginal deliveries.
A finger is inserted through the cervix and the membranes are swept (stripped) from the lower uterine segment above the internal Os through 360°.
It induces local prostaglandin formation.
It is started after 38 – 40 weeks and 2 in 3 patients may go into labor within 72 hours.
It is associated with reduced post-term pregnancy and formal induction.
Stripping of the membranes causes an increase in the activity of phospholipase and prostaglandin as well as causing mechanical dilation of the cervix, which releases prostaglandins. The membranes are stripped by inserting the examining finger through the internal cervical Os and moving it in a circular direction to detach the inferior pole of the membranes from the lower uterine segment.
Surgical Methods
Amniotomy
Technique:
- The FHR is recorded before the procedure.
- A pelvic examination is performed to evaluate the cervix & station of the presenting part. The presenting part should be well fitted to the cervix.
- The membranes are identified and a kocher is inserted through the cervical os by sliding it along the hand & fingers & membranes are ruptured.
- The nature of the amniotic fluid is recorded (clear, bloody, thick or thin, meconium).
- The FHR is recorded after the procedure.
Risks of amniotomy:
Prolapse of the umbilical cord (0.5%)
- In cord prolapse, the membrane has ruptured; in cord presentation, the membrane is still intact.
Chorioamnionitis: Risk increases with prolonged induction delivery interval
Postpartum hemorrhage: Risk is doubled compared with women with spontaneous onset of labor
Rupture of vasa previa >> FHR abnormalities.
Neonatal hyperbilirubinemia
Pharmacologic methods
Synthetic prostaglandins
Mode of action- they act on the cervix to enable ripening by a number of different mechanisms.
They alter the extracellular ground substance of the cervix and makes the cervix softer.
PG increases the activity of collagenase in the cervix also resulting in a softer cervix.
They cause an increase in elastase, glycosaminoglycan, dermatan sulfate, and hyaluronic acid levels in the cervix. A relaxation of cervical smooth muscle facilitates dilation.
Prostaglandins allow for an increase in intracellular calcium levels, causing contraction of myometrial muscle.
Risks associated with the use of prostaglandins include uterine hyperstimulation and maternal side effects such as nausea, vomiting, diarrhea, and fever.
Currently available prostaglandin analogs for the purpose of cervical ripening, dinoprostone gel (CERVIPRIME: 0.5 mg) and dinoprostone inserts (PRIMIPROST: 10 mg); Misoprostol (Cytotec: 25µg 4-6hourly).
Examples of pharmacologic agents for IOL
1. Prostaglandin E2 (dinoprostone):
It is inserted vaginally as a gel (Prepidil), as a removable tampon (Cervidil) or as a vaginal pessary. It acts on the cervical connective tissue and relaxes muscle fibers of the cervix. Dinoprostone should only be administered at hospital and the patient is expected to stay recumbent and monitored, at least, for the first 30 minutes after insertion. Contractions usually start within 60 minutes of commencing induction and peak within 4 hours. If optimal response is not achieved by 6 hours, another dose can be administered. The maximum allowed dose is 3 doses be administered per 24 hours.
Cervidil contains 10 mg of dinoprostone and provides a lower constant release of medication (0.3 mg per hour) than Prepidil does. Cervidil have the advantage of being removed more easily if uterine hyperstimulation occurs. In addition, it does not require refrigeration.
PGE2 can cause uterine hyperstimulation, fetal distress.
2. Misoprostol:
Pharmacokinetics:
- Route of administration: Oral, vaginal and sublingual route for induction. All that is required is a mucous membrane for absorption.
- Bioavailability: Extensively absorbed from the GIT
- Metabolism: De-esterified to prostaglandin F analogs
- Half-life: 20–40 minutes
- Excretion: Mainly renal 80%, remainder is fecal: 15%
- Misoprostol (Cytotec) is a synthetic PGE1 analog that has been found to be a safe and inexpensive agent for cervical ripening.
Clinical trials indicate that the safe optimal dose and dosing interval is 25 mcg intravaginally every 4-6 hours. A maximum of 4-6 doses was suggested. Higher doses or shorter dosing intervals are associated with a higher incidence of side effects, especially uterine hyperstimulation.
Misoprostol should not be used in women with previous CS because of increased rates of uterine rupture and also in women with previous precipitate labor because misoprostol itself can cause precipitate labor. Mechanical methods can be used to ripen the cervix and oxytocin used for induction in women with previous precipitate labor; mechanical methods are preferred to pharmacologic methods because they are easier to control.
The Cochrane reviewers concluded that use of misoprostol resulted in an overall lower incidence of CS. In addition, there appears to be a higher incidence of vaginal delivery within 24 hours of application and a reduced need for oxytocin augmentation
Mifepristone
Mifepristone (Mifeprex) is an antiprogesterone agent which counteracts the inhibitory effect of Progesterone on the uterus. Few studies with small number of women enrolled, have shown that women treated with mifepristone in a dose of 600 mg are more likely to have a favorable cervix and deliver within 48 to 96 hours when compared with placebo and also they these were less likely to undergo CS.
Information about fetal outcomes and maternal side effects is scarce and cannot be used to recommend the use of mifepristone for cervical ripening.
Oxytocin
It is given by IV infusion using an automated pump. Oxytocin has many advantages: it is potent and easy to titrate, has a short half-life (one to five minutes) and is well tolerated. Ideally, 10 IU Oxytocin in 1 litre of IVF recommended. It is used only for induction not cervical ripening, so the cervix must have been ripened e.g. by mechanical methods before infusion. Oxytocin infusion should not be given to a woman with an intact membrane, it increases the risk of embolism especially amniotic fluid embolism.
5 IU of oxytocin in 500 mL 5% dextrose can also be used.
Usually titrated with the uterine contractions till adequate contractions are established i.e. 3 contractions/10 minutes, each lasts between 45-60 seconds e.g. 10, 20, 30… 60 or 15, 30, 45, 60 drops/min.
Incremental interval should be 30 or 45 minutes.
If at 60d/min contractions remain inadequate, discard the solution and prepare a higher concentration e.g. 10IU in 500ml of 5% dextrose.
The ideal fluids are
- Ringers lactate
- Normal saline
- 5% dextrose saline
This protocol have the advantage of less hyperstimulation but with long induction delivery interval.
Oxytocin Protocol:
If infusion volumes were found to be excessive, prepare double strength solution.
If no progress occurred after 8–12 hours of starting induction, either discontinue the oxytocin and reapply a cervical ripening agent or re-initiate oxytocin the next day.
Continuous electronic FHR monitoring during induction is essential to monitor fetal response to labor and uterine response to the inducing agent. If severe FHR abnormalities or hyperstimulation occurred, decrease/discontinue the oxytocin infusion.
Side effects of oxytocin use:
Uterine hyperstimulation and subsequent FHR abnormalities.
Uterine rupture.
Water intoxication may occur with high concentrations of oxytocin infused with large quantities of hypotonic solutions. Therefore, AVOID prolonged administration and infusion of fluids in any 10 hours should not exceed 1500 ml. A rapid intravenous injection of oxytocin may cause hypotension
note
Monitoring during IOL
- Ideally, a one-one monitoring i.e. 1 midwife/doctor to 1 patient.
- Continuous electronic fetal monitoring is recommended.
- Regular evaluation as at when due or otherwise indicated.
- Early detection and correction of complications is of utmost importance.
Uterine hyperstimulation
STOP oxytocin
Give IVF 500mL of N/S stat
Nurse woman in left lateral position, monitor FHR every 5 minutes.
Instrumental delivery can be used to quickly deliver the baby if the woman is fully dilated.
Intravenous tocolytic
Expedite delivery through EMCS.
FHR abnormality
STOP oxytocin
IVF 500mL N/S stat
Nurse woman in LLP
Administer oxygen to improve oxygen available at the placenta bed
Monitor FHR every 5 minutes
If no improvement, expedite delivery through EMCS.
Wise conduct of induction is an important tool in Obstetric practice, injudicious use of the agents can result in a catastrophe.
We should be familiar and able to carry out this important procedure.
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.