What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
Definition:
Maternal Mortality is a death of a woman while pregnant or within 42 days of a termination of a pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental and incidental causes [WHO, 1977].
Implications of Definition:
Duration and site of pregnancy does not matter.
Deaths in early pregnancy from abortions and ectopics are maternal deaths.
Classification of maternal deaths into direct and indirect causes and exclusion of accidental and incidental causes.
A Maternal Near-Miss Case:
Defined as “a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy”.
Maternal Mortality Ratio:
Maternal deaths/livebirths x 100,000.
Actually, it is a ratio of maternal deaths (D) to live births (B) (D/B).
It is expressed as number of deaths per 100,000 live births [or as per 1000 where it is low]
Range for Nigeria is 3 - 12 per 1000.
Average [814 per 100,000]
Worldwide MM is 211 per 100,000 live births
Largely preventable and broadly divided into 4 groups:
- Medical factors
- Socio-cultural factors
- Health service factors
- Reproductive factors
1. Medical factors
Unsafe Abortion:
Abortion is widespread, occurs irrespective of age, marital status, religion, rural and urban etc.
The marked contradictions between the level of information and knowledge about contraception and the use of contraception reveal a need for integration of information, education and care in reproductive health services.
Abortion is being practiced under inadequate conditions and, even though it is most often performed by health personnel (and particularly physicians), there are physical and psychological consequences.
Only 57% of women who had abortions received counseling on family planning.
NEED FOR MANAGED CARE, FP COUNSELLING, EMERGENCY CONTRACEPTION.
2. Socio-Cultural & Economic Causes
Low status of women
Poverty
Poor nutrition [in childhood, adolescence and adulthood]
Ignorance/illiteracy
Religious beliefs [that act as barriers to utilization of available health services]
Harmful traditional practices [e.g. teenage marriages]
3. Health Service Causes
Too numerous to enumerate:
Lack of access to essential obstetric care
Lack of access to family planning [fp] counselling and service
Lack of drugs, blood, equipment, essential materials, instruments, consumables etc. in hospital
Non-availability of health workers on essential duties
Deficient transportation, communication and utility (power, water etc.) facilities.
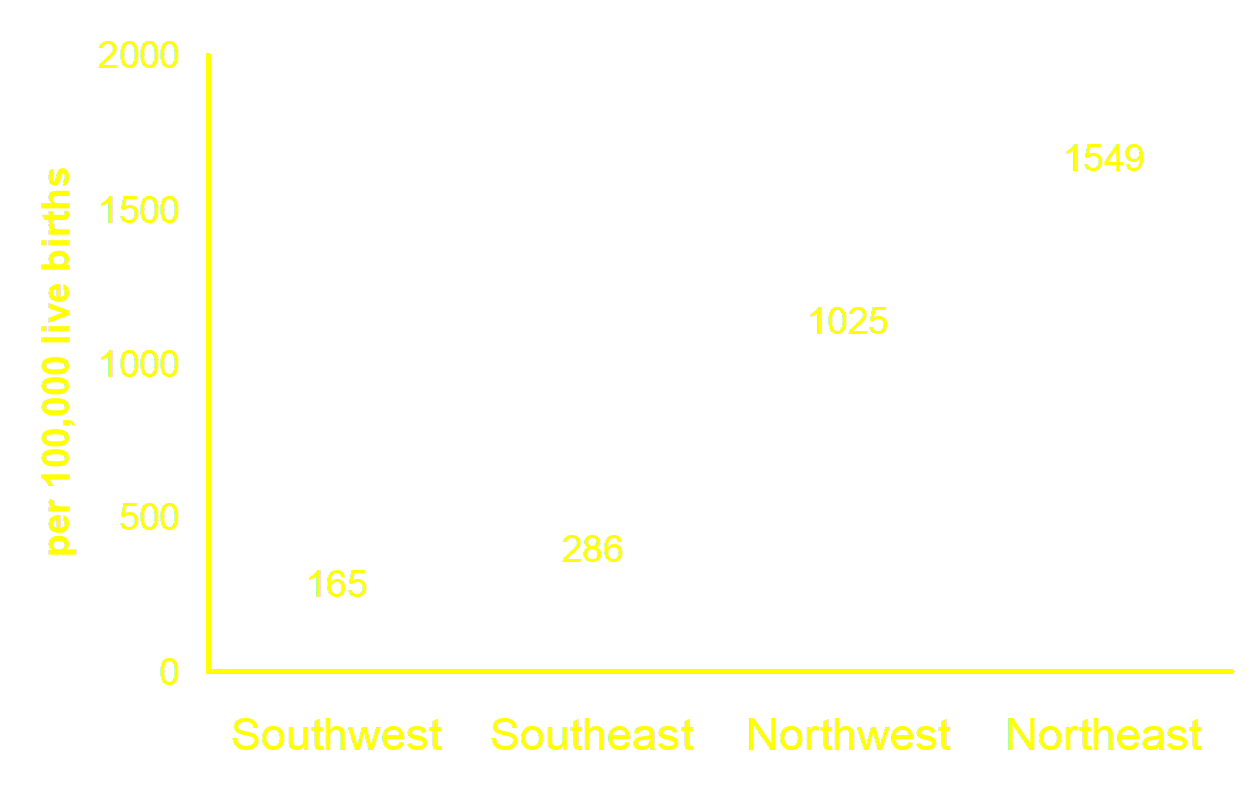
4. Reproductive Health Causes
A number of studies have shown that certain groups of women are at increased risk of maternal mortality. They include:
Too young [<18 years]
Too old [> 35 years]
Too many [having 5 or more deliveries]
Too frequent [having spacing of their deliveries less than 2 years apart]
Too sick [pregnancies contraindicated or at very high risk to life]
Direct Causes of MM (75—80%)
Haemorrhage (25%)
Infection/Sepsis (15%)
Eclampsia/high blood pressure (12%)
Unsafe abortion (13%)
Obstructed labour/and or prolong labour (8%)
Other (8%)
Indirect Causes of MM (20—25%)
HIV/AIDS
Hepatitis
Diabetes
Malaria and/or anaemia
Malaria is the leading indirect cause of MM in sub-saharan Africa.
(why women & children die)
1st Delay
In the Home & Community:
- Lack of information (inadequate knowledge) about pregnancy and labor complication signals.
- Cultural barriers.
2nd Delay
Inability to access health facility:
- Poor siting of health facilities
- Poor roads and communication network
- Poor community support
3rd Delay
Between arrival and accessing service at Health Facility:
- Inadequate skilled attendants.
- Inadequate equipment and supplies.
Family planning (FP)
Improved Antenatal Care
Essential Obs. Care
Blood banking facility
Clean and safe delivery
Postpartum care and counseling
Abortion care
Human right advocacy
Referral networks
Transportation facility
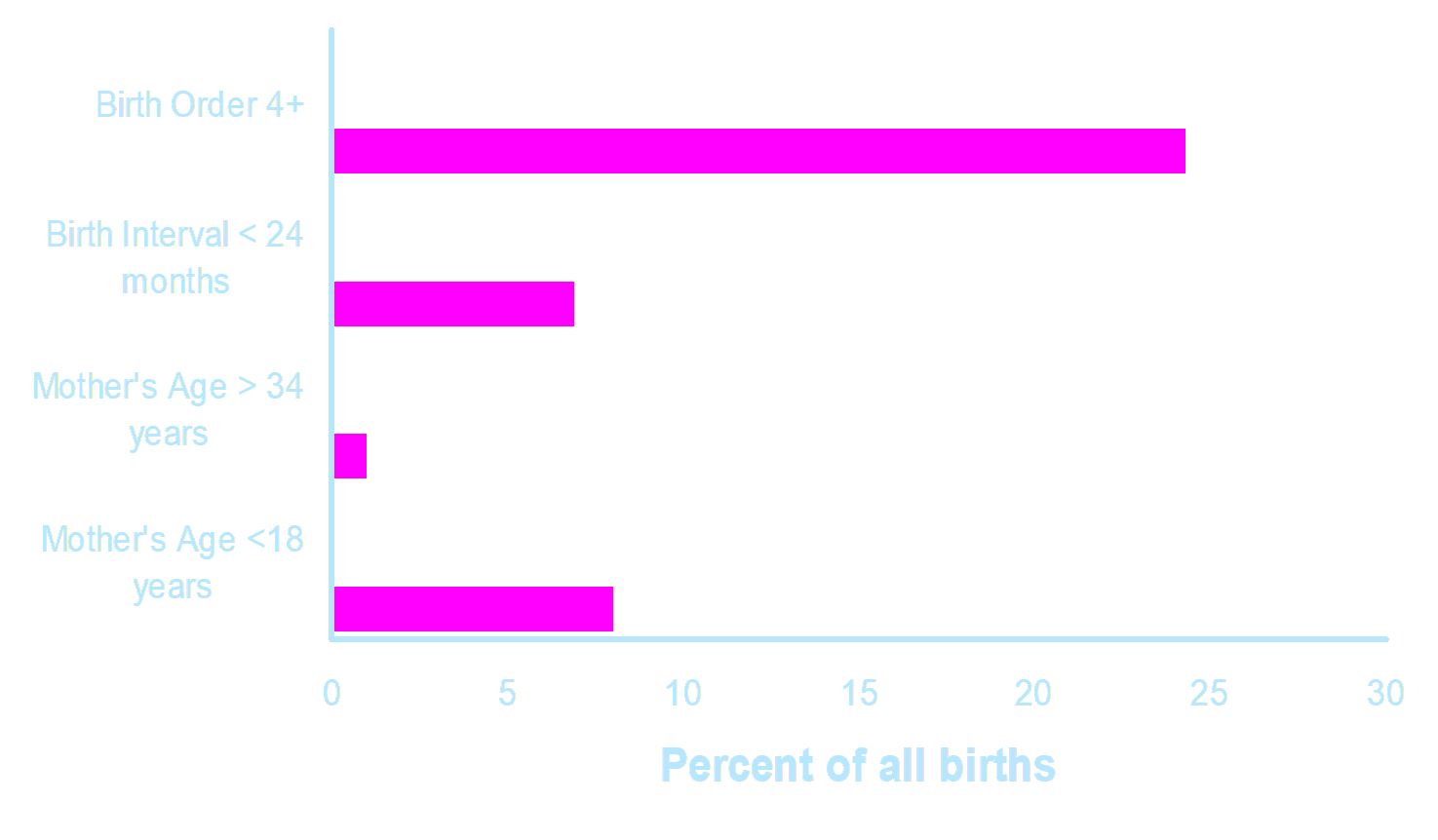
The importance of FP in reducing MM
At least half a million women die each year of pregnancy-related causes. Ninety-nine percent live in developing countries. Two approaches can reduce these deaths. First, make pregnancy and delivery safer once women become pregnant; second, reduce the number of pregnancies through family planning. Family planning reduces maternal mortality in several ways.
At the individual level, family planning reduces the number of times a woman becomes pregnant. Generally speaking, women of higher parity face greater risks in pregnancy. For example, a woman who has been pregnant six times has twice the risk of dying a maternal death as a woman who has been pregnant only three times.
Family planning reduces the number of unintended and unwanted pregnancies. Unwanted pregnancies are far more likely to end in induced abortion, and are far less likely to receive adequate prenatal care than wanted pregnancies. In some situations, abortions account for up to half of all pregnancy-related deaths. The potential for family planning to reduce these deaths is very great.
At the national level, family planning reduces the number of pregnancies and births. Even without any improvement in obstetric care, a 10% reduction in the number of pregnancies will produce a 10% (or greater) reduction in the number of maternal deaths.
Family planning can be targeted to reduce the number of pregnancies to women in groups at increased risk of maternal death, that is women who are too young (< 20), too old (>35 or >39), or women who are high parity (more than 5 previous births).
By far the most important way of reducing maternal deaths is simply by reducing the number of pregnancies. By itself, this is very effective. But it is important to pay simultaneous attention to improving obstetric care. Most women want to have at least two children, and they should have good quality care during pregnancy and for delivery. Ideally, these two interventions -- family planning and obstetric care -- should go hand-in-hand.
An important point to notice in the table is that, at least in the study area, it is far more effective (in terms of preventing maternal mortality) to prevent births to young (< 20) women than to prevent births to older women. Only 2.5% of the deaths and 2.1% of the births in Matlab occurred to women older than 39, but 32% of the deaths and 21% of the births occurred to women younger than 20; younger women are clearly at increased risk of dying in childbirth and during pregnancy.
The greatest impact of family planning on maternal mortality is for those women who are less 20 years of age. While it is a sensitive issue in many cultures, delaying pregnancy by increasing family planning use among both married and unmarried women < 20 could save many lives.
In countries where fertility is already low, the impact on maternal mortality of expanding access to family planning will not be great. There is one important exception to this; where fertility is low because of widespread use of abortion, family planning can save lives by preventing abortions.
Essential Obstetric Care
Essential obstetric care is the term used to describe the elements of obstetric care needed for the management of normal and complicated pregnancy, delivery and the postpartum period.
Essential Obstetric Care is defined for two different levels of the health care system:
- Basic essential obstetric care
- Comprehensive essential obstetric care
Basic essential obstetric care services at the health center level should include at least the following:
- Parenteral antibiotics
- Parenteral oxytocic drugs
- Parenteral sedatives/anti-convulsants for eclampsia
- Partograph monitoring
- Manual removal of placenta
- Manual removal of retained products
Comprehensive essential obstetric care services at the district hospital level (first referral level) should include all the above plus:
- Surgery
- Anesthesia, and
- Blood transfusion.
- AVD – Forceps or Vacuum
These essential obstetric functions are vital to manage the five most important causes of maternal deaths: sepsis, haemorrhage, eclampsia, obstructed labour and abortion.
Actions Required:
Promote women’s health and safe motherhood to achieve a rapid and substantial reduction in maternal morbidity and mortality.
Reduce greatly the number of death and morbidity from unsafe abortion.
Improve the health and nutritional status of women, especially of pregnant and nursing women.
Promote the role of the private sector in delivery of quality health care service, and in the production and distribution of high-quality reproductive health consumables (surgical gloves, antiseptics, instruments etc), drugs, commodities and contraceptives, which are accessible and affordable to low-income sectors of the population.
Strengthen partnership, referral linkage and collaboration between governmental, non-governmental and private sectors in promotional efforts to reduce maternal mortality
Governments are strongly encouraged to set standards for maternal/reproductive health service (24hr service, minimum staffing structure, availability of essential drugs, fluids and blood, training and re-training structure and composition etc.), and ensure compliance by governmental, non-governmental bodies.
Governments are encouraged to as a matter of urgency expand the NHIS and proffer new ways of ensuring payment of fees for private sector health care for emergency lifesaving obstetric services.
Cost-effective approach to improved maternal health care services:
Provision of basic package of maternal health care service.
Expansion of district based health care centers and first referral hospitals.
Improved management of the essential inputs to health care – drugs, personnel, equipment and infrastructure.
Essential Clinical Skills and Procedures for Managing Obstetric Complications:
Manual Vacuum Aspiration
Proper ANC examination to elicit lie, presentation, engagement etc
Proper vaginal examination to elicit cervical dilatation, position and station of presenting part, moulding, caput formation etc.
CS and types and indications
Active management of 3rd Stage
Manual removal of placenta and retained products
Delay one:
Help women and their families recognize danger signs by
- Raising awareness in communities about the signs of life-threatening complications; and
- Educating women, their partners, and their families about when and where to seek care for complications.
- Help women and their families decide to seek care by
- Encouraging families and communities to develop plans of action in case of obstetric emergencies;
- Raising women’s status so that they are empowered to make critical health decisions;
- Enhancing links between communities and health care providers;
- Improving relationships between traditional healers and skilled health care providers;
- Improving the interpersonal skills of health care providers by using information about how the community defines quality of care.
- Educating women and their families about where to seek care for complications;
- Encouraging communities to create insurance schemes to pool the costs associated with emergency care; and
- Encouraging the use of health care facilities by adolescents, single or unmarried women, and ethnic and linguistic groups who are reluctant to use services because of socio-cultural barriers.
Delay two:
Help women reach appropriate care by
- Encouraging communities to create emergency transportation plans;
- Upgrading roads and other transportation systems;
- Enhancing referral systems between communities and health care providers; and
- Establishing maternity waiting homes.
Delay three:
Make sure women receive care at health facilities by
- Upgrading the quality of care at health facilities, including improving providers’ technical and interpersonal skills, motivation, and performance;
- Establishing national protocols for treating obstetric complications;
- Training health facility staff to recognize and admit patients with life-threatening complications;
- Ensuring adequate and sustainable supplies of emergency medicines, essential equipment, blood, and staffing levels at health facilities;
- Providing 24-hour service at facilities that provide emergency obstetric care;
- Enhancing referral systems between communities and health facilities;
- Improving communication between the units that provide care in order to generate more referrals; and
- Ensuring that the national curricula for health providers include practical components about treating obstetrical emergencies.
- Reducing maternal deaths requires well-coordinated and sustained efforts. Governments and communities can work to make motherhood safer by assessing local conditions and building on existing resources and health care networks, by monitoring progress, and by helping women overcome the obstacles to receiving lifesaving care.
- Ultimately, the critical need may be one of generating sufficient political, and social will at international and national levels to overcome this avoidable tragedy.
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions