What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
Ectopic pregnancy is a term that is derived from the Greek word ektopos, meaning out of place.
Ectopic pregnancy can lead to massive hemorrhage, infertility, or death.
In the western world, the increased incidence of ectopic pregnancy has been partially attributed to improved ability in making an earlier diagnosis.
In the poorer countries like Nigeria, the higher incidences may still be associated with higher incidences of sexually transmitted infections (STIs) such as gonorrhea, chlamydia, etc. or their poor treatment.
Definition
Ectopic pregnancy is the result of a flaw in human reproductive physiology that allows the conceptus to implant and mature outside the endometrial cavity, which ultimately ends in the death of the fetus. Without timely diagnosis and treatment, ectopic pregnancy can become a life-threatening situation.
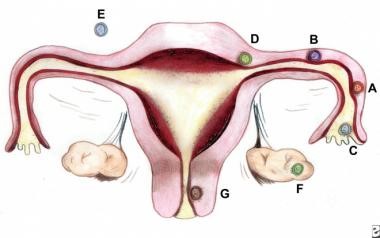
- Ampullary, 80%;
- Isthmic, 12%;
- Fimbrial, 5%;
- Cornual/Interstitial, 2%;
- Abdominal, 1.4%;
- Ovarian, 0.2%; and
- Cervical, 0.2%; Caesarean scar ectopic pregnancy (CSEP) is a rare occurrence, its frequency appears to be increasing with the increasing number of caesarean sections being performed.
Multiple factors contribute to the relative risk of ectopic pregnancy. In theory, anything that hampers or delays the migration of the fertilized ovum (blastocyst) to the endometrial cavity can predispose a woman to ectopic gestation. The following risk factors have been linked to ectopic pregnancy:
- Tubal damage - Which can be the result of infections such as pelvic inflammatory disease (PID) or salpingitis (whether documented or not) or can result from abdominal surgery or tubal ligation or from maternal in utero diethylstilbestrol (DES) exposure.
- History of previous ectopic pregnancy
- Smoking - A risk factor in about one third of ectopic pregnancies; smoking may contribute to decreased tubal motility by damage to the ciliated cells in the fallopian tubes.
- Altered tubal motility - As mentioned, this can result from smoking, but it can also occur as the result of hormonal contraception; progesterone-only contraception and progesterone intrauterine devices (IUDs) have been associated with an increased risk of ectopic pregnancy.
- History of 2 or more years of infertility (whether treated or not) - Women using assisted reproduction seem to have a doubled risk of ectopic pregnancy (to 4%), although this is mostly due to the underlying infertility.
- History of multiple sexual partners.
- Maternal age - Although this is not an independent risk factor.
The classic clinical symptom of ectopic pregnancy is as follows:
- Amenorrhea
- Abdominal pain
- Vaginal bleeding, and
- Dizziness.
Unfortunately, only about 50% of patients present with all symptoms.
Patients may present with other symptoms common to early pregnancy (e.g., nausea, breast fullness).
The following symptoms have also been reported:
- Painful fetal movements (in the case of advanced abdominal pregnancy)
- Others are: Weakness, Fever, Flulike symptoms, Vomiting, Syncope, Cardiac arrest.
The presence of the following signs suggests a surgical emergency:
- Abdominal rigidity
- Involuntary guarding
- Severe tenderness
- Evidence of hypovolemic shock (e.g., orthostatic blood pressure changes, tachycardia)
Findings on pelvic examination may include the following:
- The uterus may be slightly enlarged and soft,
- Uterine or cervical motion tenderness may suggest peritoneal inflammation,
- An adnexal mass may be palpated but is usually difficult to differentiate from the ipsilateral ovary,
- Uterine contents may be present in the vagina, due to shedding of endometrial lining stimulated by an ectopic pregnancy.
Serum β-HCG levels
In a normal pregnancy, the β-HCG level doubles every 48-72 hours until it reaches 10,000-20,000mIU/mL. In ectopic pregnancies, β-HCG levels usually increase less.
Mean serum β-HCG levels are lower in ectopic pregnancies than in healthy pregnancies.
Serial serum β-HCG levels are necessary to differentiate between normal and abnormal pregnancies and to monitor resolution of ectopic pregnancy once therapy has been initiated.
The discriminatory zone of β-HCG (i.e., the level above which an imaging scan should reliably visualize a gestational sac within the uterus in a normal intrauterine pregnancy) is as follows:
- 1500-1800 mIU/mL with transvaginal ultrasonography, but up to 2300 mIU/mL with multiple gestates
- 6000-6500 mIU/mL with abdominal ultrasonography
Absence of an intrauterine pregnancy on a scan when the β-HCG level is above the two discriminatory zones represents an ectopic pregnancy or a recent abortion.
The above represents the most modern way of using Serum β-HCG levels in the diagnosis of ectopic pregnancy.
Ultrasonography
Ultrasonography is probably the most important tool for diagnosing an extrauterine pregnancy.
Visualization of an intrauterine sac, with or without fetal cardiac activity, is often adequate to exclude ectopic pregnancy.
Transvaginal ultrasonography, or endo-vaginal ultrasonography, can be used to visualize an intrauterine pregnancy by 24 days post ovulation or 38 days after the last menstrual period (about 1 week earlier than transabdominal ultrasonography). An empty uterus on endo-vaginal ultrasonographic images in patients with a serum β-HCG level greater than the discriminatory cut-off value is an ectopic pregnancy until proved otherwise.
Color-flow Doppler ultrasonography improves the diagnostic sensitivity and specificity of transvaginal ultrasonography, especially in cases in which a gestational sac is questionable or absent.
Laparoscopy
Laparoscopy remains the criterion standard for diagnosis; however, its routine use on all patients suspected of ectopic pregnancy may lead to unnecessary risks, morbidity, and costs. Moreover, laparoscopy can miss up to 4% of early ectopic pregnancies.
Laparoscopy is indicated for patients who are in pain or hemodynamically unstable.
Only 50% of patients with an ectopic pregnancy present with the classic triad of pain, amenorrhea, and vaginal bleeding. Numerous conditions may have a presentation similar to an extrauterine pregnancy. The most common of these include the following:
- Appendicitis
- Salpingitis
- Ruptured corpus luteum cyst or ovarian follicle
- Spontaneous abortion or threatened abortion
- Ovarian torsion
- Urinary tract disease
- Intrauterine pregnancies with other abdominal or pelvic problems, such as degenerating fibroids, must also be included in the differential diagnosis.
The availability of various biochemical, ultrasonographic, and surgical modalities can aid the healthcare provider today in establishing a definitive diagnosis and differentiating among various conditions.
The role of β-HCG, ultrasound and laparoscopy has been discussed above.
Blood type, Rh type, and antibody screen should be done in all pregnant patients with bleeding to identify patients in need of RhoGAM and to ensure availability of blood products in case of excessive blood loss.
In women with normal baseline findings for liver function tests (LFTs), renal function tests (RFTs), and complete blood count (CBC) on day 1 of single- or double-dose methotrexate (MTX) treatment for sonographically confirmed ectopic pregnancies, it may not be necessary to repeat these studies, as there appears to be no significant difference between results on day 1 and day 7 for either MTX treatment protocol.
Other tests: Dilatation and curettage as well as culdocentesis/abdominal paracentesis!!!
The commonest mode of presentation in this environment is the acute, anemic patient requiring the full deployment of cardiovascular resuscitation (ABCDE). This requires a team approach as there often is the need for quick history, keeping the patient alive and at the same time operating to stop the bleeding into the abdominal cavity from the ruptured ectopic site.
Among the greatest advances in the management of ectopic pregnancy has been the development of medical management, which became available in the mid-1980s.
Therapeutic options in ectopic pregnancy are as follows:
- Expectant management
- Methotrexate
- Surgery
Expectant management
Candidates for successful expectant management should be asymptomatic and have no evidence of rupture or hemodynamic instability. Candidates should demonstrate objective evidence of resolution (e.g. declining β-HCG levels).
Close follow-up and patient compliance are of paramount importance, as tubal rupture may occur despite low and declining serum levels of β-HCG.
Methotrexate
Methotrexate is the standard medical treatment for unruptured ectopic pregnancy. A single-dose IM injection is the more popular regimen. The ideal candidate should have the following:
- Hemodynamic stability,
- No severe or persisting abdominal pain,
- The ability to follow up multiple times,
- Normal baseline liver and renal function test results.
Absolute contraindications to methotrexate therapy include the following:
- Existence of an intrauterine pregnancy
- Immunodeficiency
- Moderate to severe anemia, leukopenia, or thrombocytopenia
- Sensitivity to methotrexate
- Active pulmonary or peptic ulcer disease
- Clinically important hepatic or renal dysfunction
- Breastfeeding
- Evidence of tubal rupture
Other Drugs: Potassium chloride, hyperosmolar glucose, mifepristone (RU 486), and prostaglandins. These therapies are experimental at present.
Surgical treatment
Laparoscopy has become the recommended surgical approach in most cases. Laparotomy is usually reserved for patients who are hemodynamically unstable or for patients with cornual ectopic pregnancies; it also is a preferred method for surgeons inexperienced in laparoscopy and in patients in whom a laparoscopic approach is difficult.
Salpingostomy - Within the last 2 decades, a more conservative surgical approach to unruptured ectopic pregnancy using minimally invasive surgery has been advocated to preserve tubal function. The conservative approaches include linear salpingostomy and milking the pregnancy out of the distal ampulla.
Salpingectomy - The more radical approach includes resecting the segment of the fallopian tube that contains the gestation, with or without re-anastomosis.
Morbidities and mortalities can also result apart from reproductive outcomes.
But a good number of cases result in good prognosis if professionally managed.
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions