What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
Dysfunctional uterine bleeding (DUB) is classically defined as abnormal (excessively heavy, scanty, prolonged, frequent or infrequent) bleeding of uterine origin that is not caused by pregnancy or recognizable pelvic or systemic disease.
Up to 20% of women will experience irregular cycles in their lifetimes.
It is a diagnosis of exclusion i.e. it is only diagnosed after the most probable causes have been ruled out by appropriate investigations. Causes such as:
- Pregnancy
- Medications
- Iatrogenic causes
- Genital tract pathology
- Malignancy
- Systemic diseases e.g. bleeding disorders
- Anovulatory
- Ovulatory
Approximately 90% of dysfunctional uterine bleeding cases result from anovulation, and 10% of cases occur with ovulatory cycles.
Anovulatory DUB
Usually results from disordered functioning of the hypothalamic-pituitary-ovarian (HPO) axis.
Occurs most often in women at the extreme ends of their reproductive lifetime.
Both perimenarchal and perimenopausal women have several anovulatory cycles per year, it is therefore a common problem in adolescent females as well as elderly women.
Other causes/risk factors for anovulatory uterine bleeding include-
- Excessive exercise
- Emotional stress
- Eating disorders (bulimia and anorexia)
- Obesity
- Polycystic ovarian syndrome (PCOS)
- Hyperprolactinemia
- Thyroid disease
Most cannot be classified as DUB, some are gray areas.
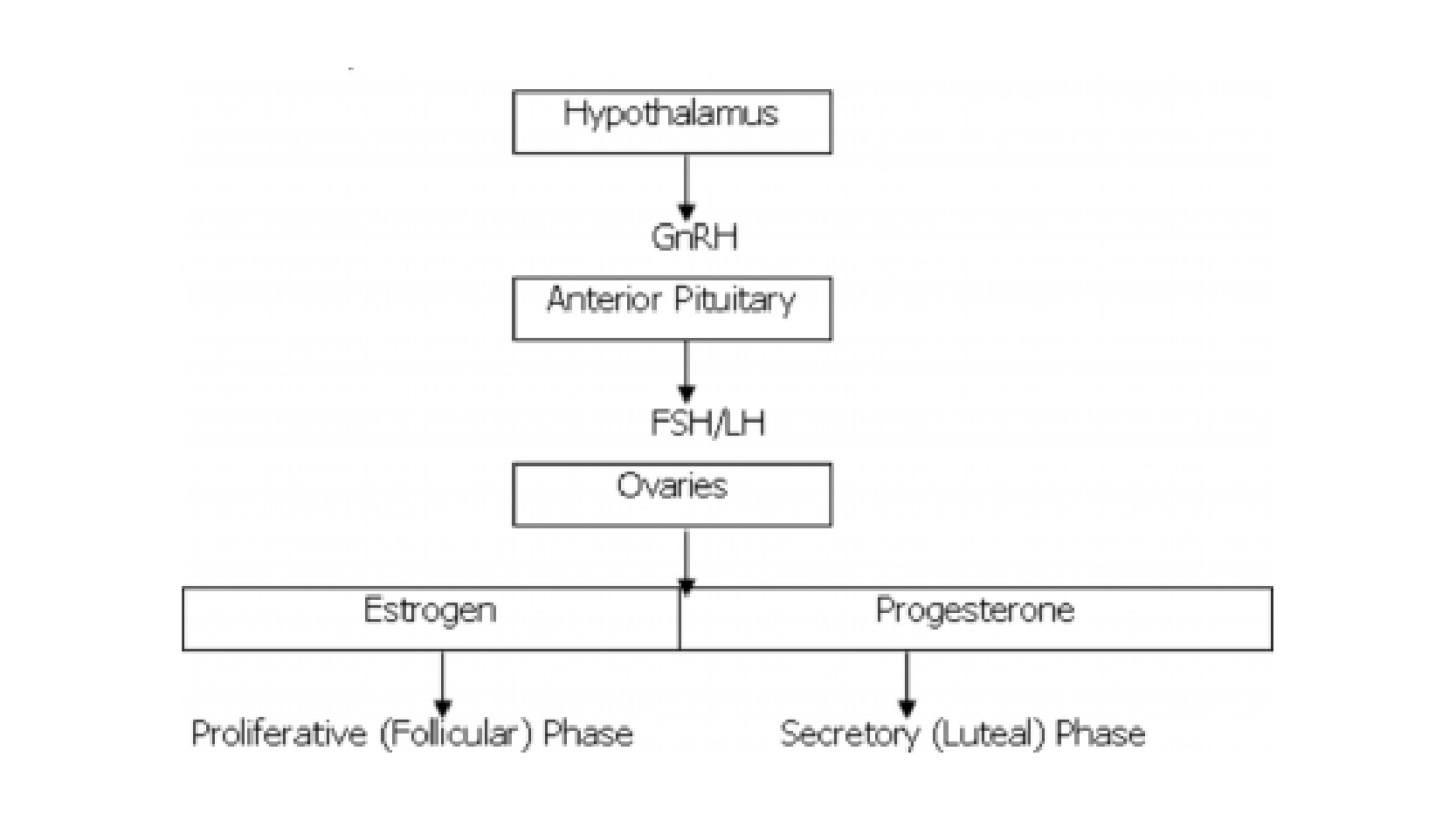
Hypothalamic-Pituitary-Ovarian (HPO) axis
GnRH is released from the hypothalamus in pulses which vary depending on the phase in the menstrual cycle.
GnRH pulse frequency is approximately once per 90 min in the follicular phase.
The pulses are less frequent in the luteal phase, occurring approximately once in 4 h.
GnRH acts on the anterior pituitary through the hypothalamohypophyseal portal system to cause release of the gonadotropins - LH and FSH. These in turn act on the ovary to cause release of estrogen and progesterone.
Disorders that slow GnRH pulsatility, such as anorexia nervosa, result in failure of secretion of pituitary gonadotropins (LH and FSH) and a state of hypogonadal hypogonadism with failure of follicular development and amenorrhea.
Less severe reductions in GnRH pulse amplitude and frequency result in diminished FSH and LH with some follicular stimulation but not enough to result in ovulation but estradiol is secreted. This may occur in stress, hyperprolactinemia, excessive exercise or may be idiopathic.
An understanding of the normal cyclic fluctuations of the 2 gonadotropins (i.e., luteinizing hormone [LH], follicle-stimulating hormone [FSH]) and the primary female reproductive hormones (i.e., estrogen, progesterone) helps clarify the derangements associated with anovulation.
Pathophysiology of Anovulatory DUB
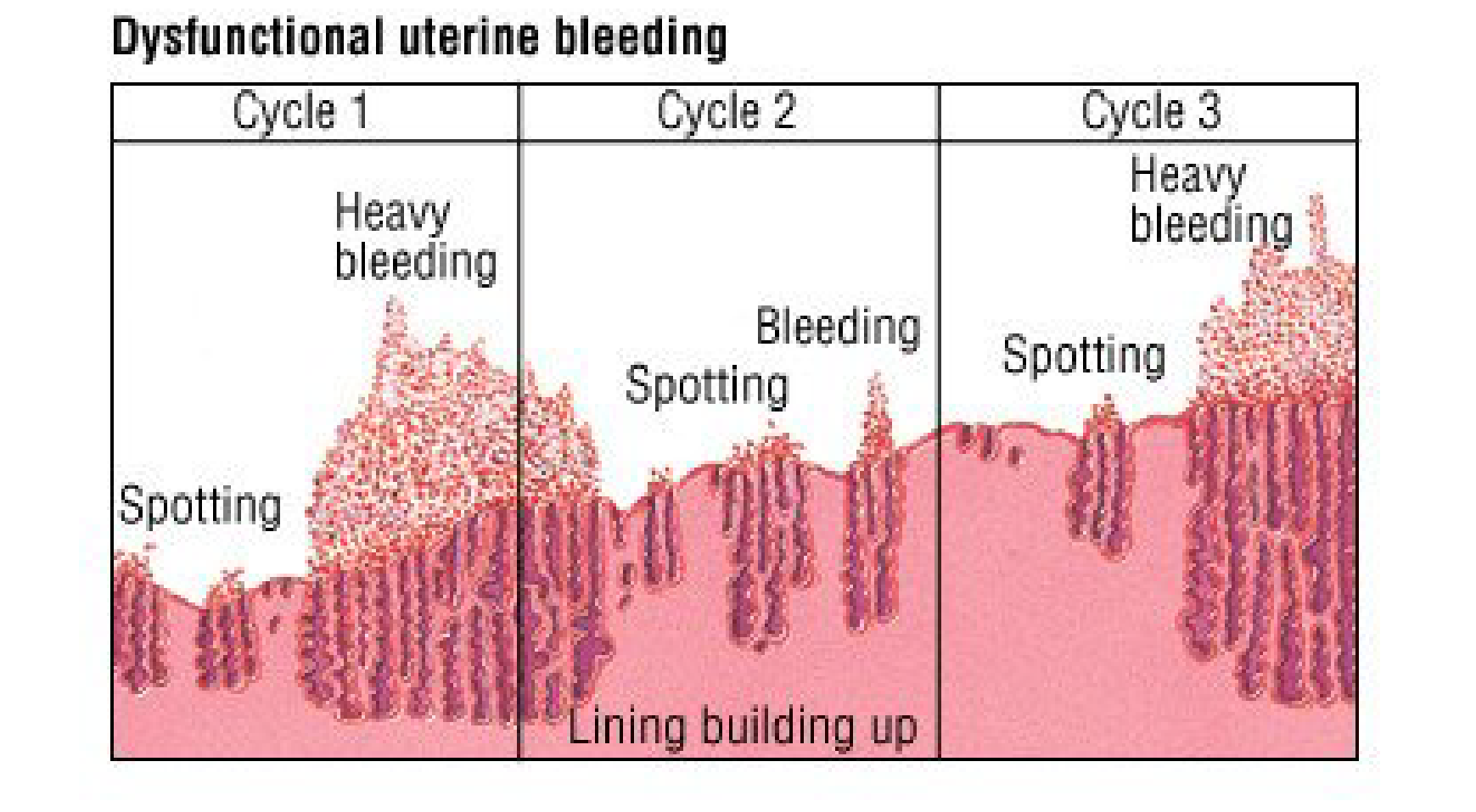
With anovulation, estrogen levels rise as usual in the early phase of the cycle and because there is no ovulation, a corpus luteum never forms and progesterone is not produced.
There is a continuous unopposed estrogenic stimulation of the endometrium. Theendometrium as a result moves into a hyperproliferative state, ultimately outgrowing its blood supply.
This leads to irregular sloughing of the endometrium and excessive bleeding from spiral arteries that have not undergone physiological senescence.
Ovulatory DUB
This type of bleeding occurs cyclically, and thought to originate from defects in the control mechanisms of menstruation.
Occurs in women of reproductive age.
Occurs less commonly.
Normal menstrual cycle
The normal cycle is 28-29 days (range of 21-35d).
Normal menstrual flow lasts 3-7days.
Average total blood loss of 25-69 mL. Flow longer than 7 days and blood loss exceeding 80 mL is considered abnormal.
The normal cycle is characterized by sequential growth, maturation and eventual sloughing of the endometrial mucosa.
This is produced by the cyclic release of estrogen and progesterone from the ovary and is orchestrated by the HPO axis.
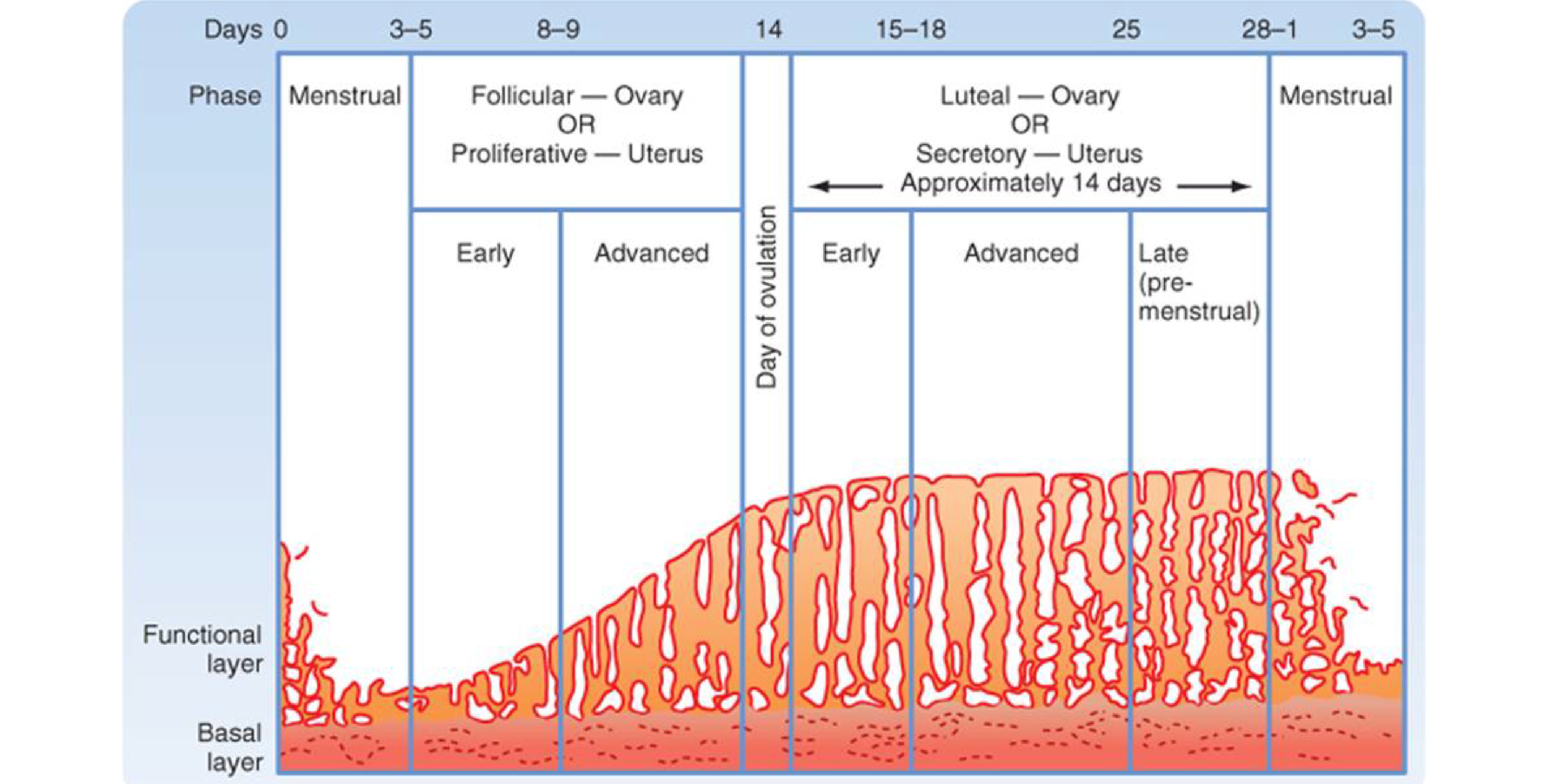
FSH stimulates ovarian follicle development and the subsequent production of estrogen, primarily estradiol.
The endometrium, under the influence of estrogen, undergoes proliferation.
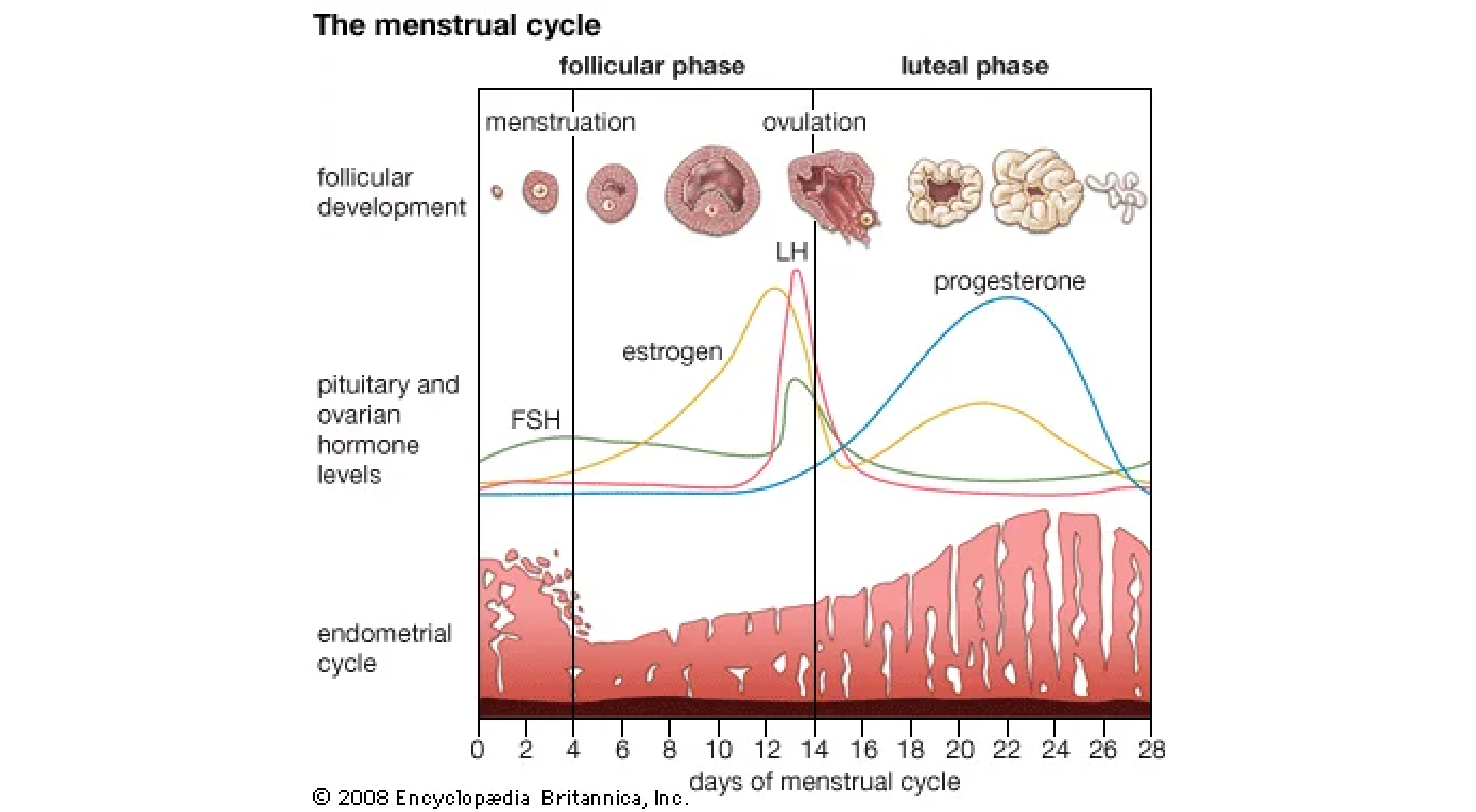
LH levels abruptly peak on day 12 or 13 in positive response to rising estrogen level. The LH surge stimulates-
- Ovulation (on or about day 14), and
- Conversion of the ovulatory follicle to corpus luteum, which is responsible for progesterone production.
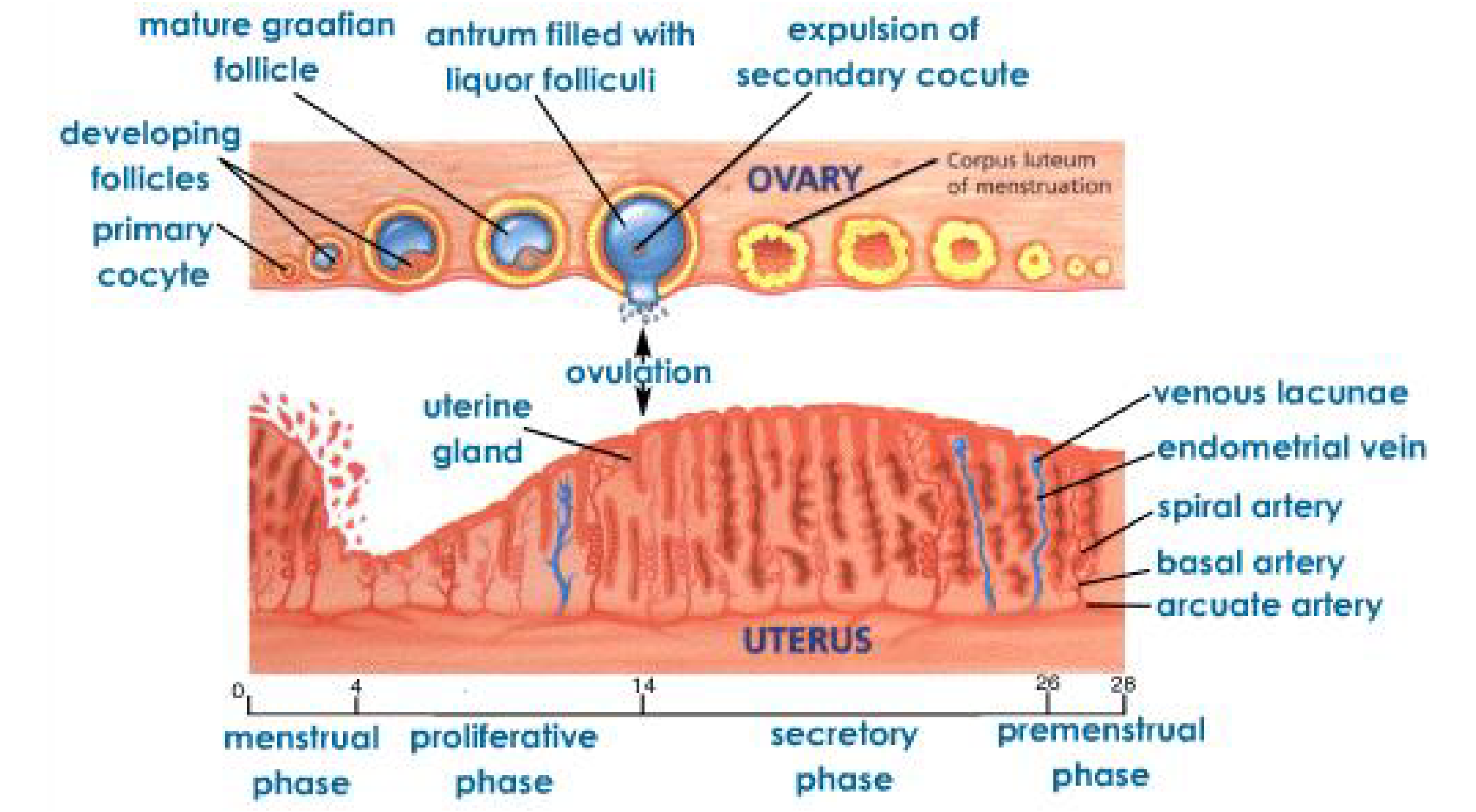
Under the influence of progesterone, the endometrium is converted to a secretory state in preparation for implantation if fertilization of the ovum should occur. Progesterone is produced only if ovulation occurs.
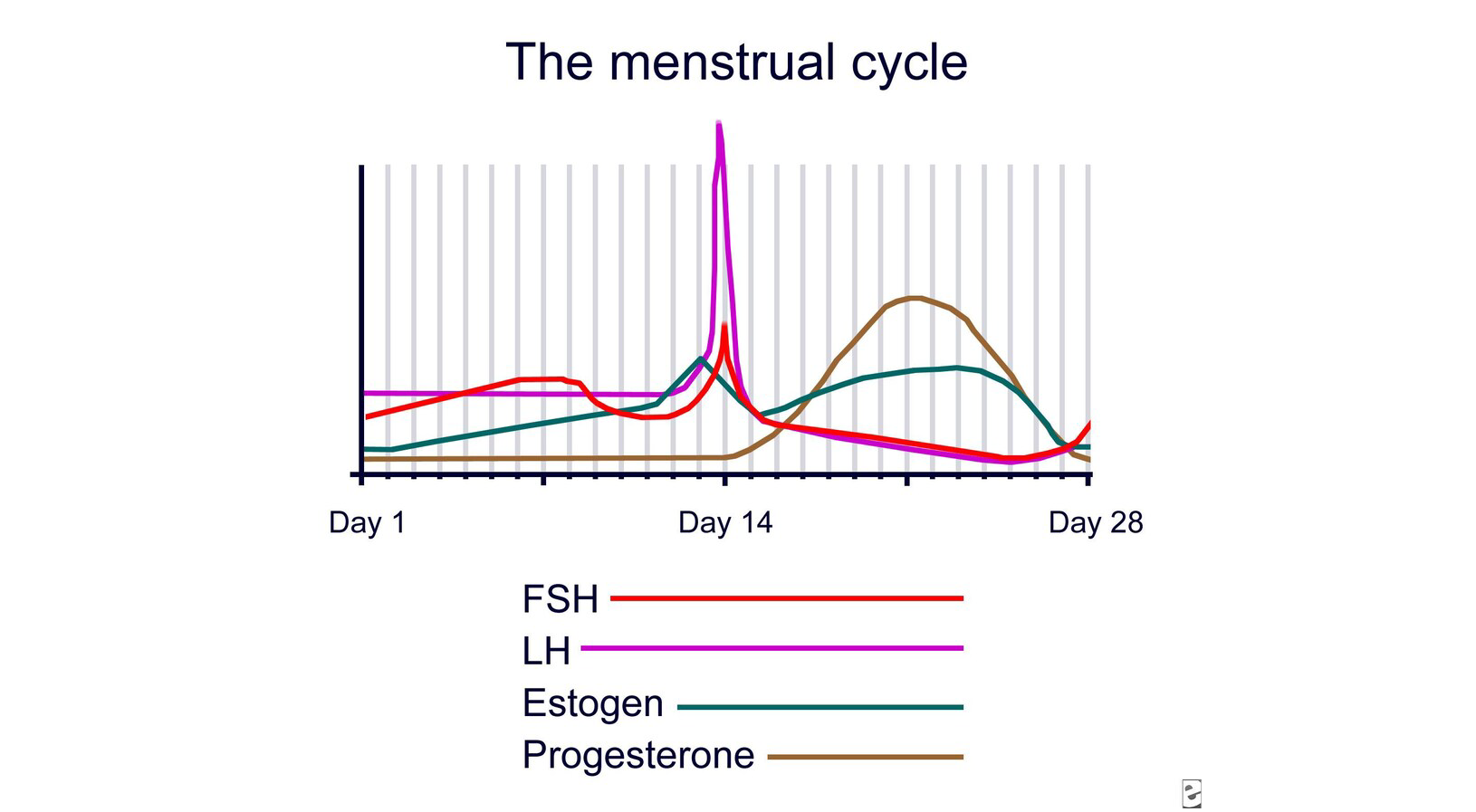
As LH levels drop (in the absence of fertilization, production of human chorionic gonadotropin [HCG] by the developing conceptus does not occur), the corpus luteum regresses, estrogen and progesterone levels plummet, and the endometrium deteriorates and is sloughed.
Pathophysiology of Ovulatory DUB
Bleeding occurs cyclically.
There is an increased rate of blood loss resulting from vasodilatation of the vessels supplying the endometrium due to decreased vascular tone, and prostaglandins have been strongly implicated.
Therefore, these women lose blood at rates about 3 times faster than women with normal menses.
note
Prostaglandins involved in menstruation
- PGF2α: Vasoconstrictor and weak platelet aggregator.
- PGE2: Vasodilator and weak platelet anti-aggregator.
- PGD: Vasodilator and smooth muscle relaxant.
- PGI: Potent vasodilator and inhibitor of platelet aggregation.
- TXA2: Potent vasoconstrictor and platelet aggregator.
In women with normal blood flow the order of production of prostaglandins by the secretory endothelium is PGF2α/PGE2/PGD.
Increased amount of PGI (prostacyclin) are produced in the myometrium of DUB patients due to increased production of endoperoxidases.
Common terminologies for abnormal menstruation
Menorrhagia: heavy bleeding, including prolonged menstrual periods (bleeding that lasts more than 7 days), or excessive bleeding (blood loss of greater than 80 ml per period) during a normal length period.Regular cycles, prolonged duration, excessive flow.
Metrorrhagia: bleeding at irregular intervals, particularly between expected menstrual periods. Frequent and irregular cycles.
Menometrorrhagia: prolonged or excessive uterine bleeding that occurs irregularly and more frequently than normal. Irregular, prolonged, excessive.
Hypermenorrhea: a menstrual period with excessively heavy flow. Regular, normal duration, excessive flow.
Polymenorrhea: frequent regular cycles that is shorter than 21 days.
Oligomenorrhea: Infrequent cycles. Uterine bleeding at regular intervals from 35 days to 6 months.
Amenorrhea: primary amenorrhea is the failure of menses to occur by age 16, in the presence of normal growth and secondary sexual characteristics. Secondary amenorrhea is the cessation of uterine bleeding in a post-menarchial girl or a reproductive-aged woman for > 6 months.
Postmenopausal bleeding: uterine bleeding that occurs more than 1 year after the last menses in a woman with ovarian failure.
Patients may present with a chronic light flow in the form of irregular, prolonged, or intermenstrual bleeding that is a nuisance but not a significant health threat.
Alternatively, patients can present with acute torrential hemorrhage requiring immediate medical attention.
Abortion: Threatened, incomplete. The most common cause of abnormal uterine bleeding during the reproductive years is abnormal pregnancy.
Ectopic Pregnancy
Uterine Fibroids
Pelvic inflammatory disease (PID)
Polyps
Adnexal Tumors: functional ovarian tumors
Cervical cancer- it is the most common gynecological cancer affecting women of reproductive age in the world.
Cervicitis
Vaginitis
Chlamydial genitourinary infections
Endometrial carcinoma
Endometriosis
Endometritis
Gestational trophoblastic neoplasia
Hyperprolactinemia
Hyperthyroidism
Hypothyroidism
Ovarian polycystic disease
Clotting disorders
Conditions affecting liver metabolism of estrogen can be associated with abnormal uterine bleeding.
Coagulation factors deficiency e.g. Von Willebrand disease and factor XI deficiency initially might manifest during adolescence.
Primary or secondary thrombocytopenia can be factors in the mature patient.
- Hematocrit/PCV
- Pelvic ultrasound: In obese patients with suboptimal pelvic examination, suspected ovarian or uterine pathology, to examine the status of the endometrium etc.
- Pregnancy test/Human chorionic gonadotropin.
- High vaginal swab/Endometrial swab for MCS
- Saline-infusion sonohysterography is also very useful in evaluating for intracavitary (submucosal) fibroids and endometrial polyps.
- Pap smear.
- Endometrial biopsy to rule out endometrial hyperplasia or cancer.
- Thyroid function test
- Hormonal assay: A hormonal complete evaluation in women with signs of hyperandrogenism, such as in polycystic ovarian syndrome, 21 hydroxylase deficiency, or ovarian or adrenal tumors.
- Women in menopausal transition usually can be followed without an extensive hormonal evaluation.
- Liver function test.
- Medical
- Surgical
Medical treatments
Drugs used to treat DUB:
- Estrogens
- Progestins
- Androgens
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Ergot derivatives
- Antifibrinolytics
- Gonadotropin-releasing hormone (GnRH) agonists
- Desmopressin has been used to control bleeding when associated with diagnosed bleeding disorders.
Combined oral contraceptives
COCs contain both estrogen and progestins.
With COCs pills, bleeding usually is controlled within the first 24 hours, as the overgrown endometrium becomes pseudodecidualized, reestablish predictable bleeding patterns, decrease menstrual flow, and lower the risk of anemia.
Additional benefits, include decreased dysmenorrhea and ovarian cancer prophylaxis.
Estrogens
Tablets or injections
E.g. IV Premarin
Useful for acute bleeding.
25 mg IV q4 hours(every 4 hours) until bleeding slows.
Causes nausea, breast tenderness.
Give slowly or can cause vasovagal reaction or LOC.
Must give progestins for 7- 10 days after and then will have withdrawal bleed or start continuous OCPs.
Progestins
Mainly indicated in patients with anovulatory bleeding to reverse the effects of estrogen mediated endometrial proliferation and induce endometrial maturation.
Cyclic progestin for 10 days per month using medroxyprogesterone acetate (10 mg/d) or norethindrone acetate (2.5-5 mg/d) provides predictable uterine withdrawal bleeding, but not contraception.
Non-steroidal anti-inflammatory drugs
Blocks formation of prostacyclin, an antagonist of thromboxane, which is a substance that accelerates platelet aggregation and initiates coagulation. Prostacyclin is produced in increased amounts in menorrhagic endometrium. NSAIDS thus effectively decrease uterine blood flow.
Examples include Mefenamic acid and Naproxen.
GnRH agonists
Induces postreceptor effects, which suppress gonadotropin release, with resultant hypogonadism resulting in amenorrhea, thus breaking cycle of abnormal bleeding in anovulatory patients.
Should not be used for more than 6months without adding a back-up therapy.
Prolonged use is associated with osteoporosis and other postmenopausal side effects.
Antifibrinolytics
At the onset of menses, secretory endometrium contains a high concentration of plasminogen activator.
A reduction in menstrual blood loss has been demonstrated in some ovulatory patients taking ε-aminocaproic acid (EACA) or aminomethylcyclohexane-carboxylic acid (AMCHA) tranexamic acid, both potent antifibrinolytics.
Androgens
Androgens have been used to treat mild to moderate bleeding, particularly ovulatory DUB, they function by altering endometrial tissue so that it becomes inactive and atrophic.
They offer no real advantage over other regimen, can cause irreversible signs of masculinization.
They are seldom used again.
They might stimulate erythropoiesis and clotting deficiency.
Examples are Danazol (Danocrine) and Isoxazole, derivative of 12 alpha-ethinyl testosterone
Surgical treatments
Surgical measures are reserved for situations when medical therapy has failed or is contraindicated.
D&C can be used to clear the endometrium in in a patient who fails to respond to hormonal management and also to obtain a biopsy but this is not commonly done anymore.
Hysteroscopy will aid in the treatment of endometrial polyps or the performance of directed uterine biopsies.
Abdominal or vaginal hysterectomy might be necessary in patients who have failed or declined hormonal therapy, have symptomatic anemia, and who experience a disruption in their quality of life from persistent, unscheduled bleeding.
Endometrial ablation is an alternative for those who wish to avoid hysterectomy or who are not candidates for major surgery. Ablation techniques are varied and can employ laser, rollerball, resectoscope, or thermal destructive modalities.
- Pretreat the patient with an agent, such as leuprolide acetate, medroxyprogesterone acetate, or danazol, to thin the endometrium.
- An endometrial biopsy is needed before ablation.
- The ablation procedure is more conservative than hysterectomy and has a shorter recovery time.
- Endometrial ablation is not a form of contraception. Some studies report up to a 5% pregnancy rate in post-ablation procedures.
Some patients may have persistent bleeding and require repeat procedures or move on to hysterectomy.
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.