What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
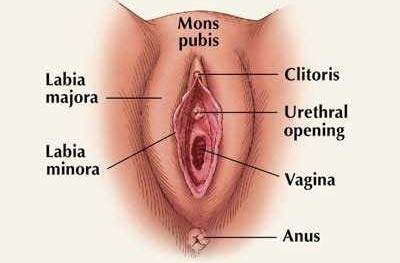
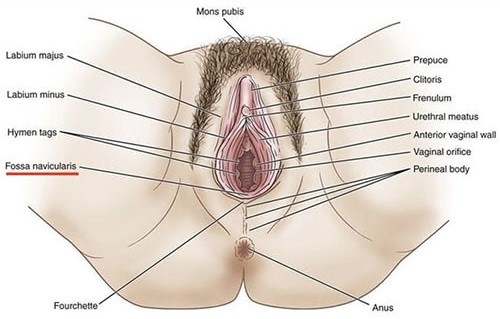
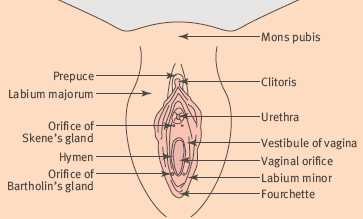
The vulva consists of the-
- Labia majora
- Labia minora
- Mons pubis
- Clitoris
- Vestibule (with the greater/lesser vestibular gland)
The vagina tubular muscular organ, upper blind edge attached to the vagina at the vault.
Varies but can be divided into four:
- Dermatoses not unique to vulva
- Inflammatory vulva dermatoses
- Benign ulcers, cysts, and tumors
- Vulval atypias (previously vulval dystrophies)
Dermatoses not unique to vulva
Vulva manifestation of systemic diseases-
- Dermatological diseases:
- Dermatitis medicamentosa, a local reaction to systemic drug.
- Psoriasis: chronic relapsing dermatosis, also in the scalp, trunk. Thick area of discolored skin covered with scales. Treated with topical corticosteroid.
- Bullous eruptions due to pemphigus vulgaris (autoimmune disease).
- Obesity
- Acanthosis nigricans: hyper-pigmented papillomatous hypertrophic lesions.
- Intertrigo: inflammatory reaction in genitocrural folds.
- Diabetes mellitus
- Diabetic vulvitis- chronic
- Necrotizing fascitis: rapidly spreading subcutaneous infection, it can follow episiotomy or trauma.
Lichenification- skin lesion characterized by thickening, hyperpigmentation and exaggerated skin lines.
Seborrheic and atopic dermatitis.
Contact dermititis-
- From local irritants e.g. vaginal discharge, menstrual fluids, urine and feces, retention of secretions by underwear.
- Prevention is by good hygiene, loose cotton underwear, avoidance of chemical irritants for douching or hygienic sprays.
Inflammatory vulva dermatoses
Vulval candidiasis
Staphylococcal folliculitis
Secondary irritative vulvitis
Hydradenitis suppurativa- a disorder of the terminal follicular epithelium in the apocrine gland-bearing skin. These lesions most commonly occur in intertriginous areas.
Benign ulcers, cysts & tumors
Ulcerative lesions
Behcets syndrome- a multisystemic inflammatory disorder that predominantly affect the venous system and it is characterized by a triple symptom complex of recurrent oral aphthous ulcers, genital ulcers, and uveitis.
Herpes simplex- ulcer usually found in mouth and vulva.
Syphilis- painless ulcer.
Chancroid (H. ducreyi)
Granuloma inguinale (Klebsiella granulomatis)
Benign cysts
Bartholin cyst/abscess-
- The Bartholin ducts are 2cm ducts found at 5 and 7 o’clock at introitus.
- They can become obstructed due to gonococcal infection or trauma from mediolateral episiotomy
- When the Bartholin’s gland duct orifice becomes obstructed, the glands produce a build-up of mucus. This build-up leads to a cystic dilatation of the duct and cyst formation. Infection of this cyst is likely to result in Bartholin’s gland abscess.
- Swelling may be up to 1—8 cm in diameter.
- Often affect reproductive age women; if > 40 years, rule out adenocarcinoma.
- Causes pain, superficial dyspareunia.
- Treatment is drainage by marsupialization, insertion of a word catheter for 3—4 weeks. Using incision and drainage can cause recurrence. The cyst can also be excised in recurrent cases or in patients older than 40 years.
Sebaceous cysts
- Caused by blocking of the duct of multiple sebaceous glands of the hair-bearing surface of the vulva.
- Painless, involves the labia majora
- May become secondarily infected
- Treatment is by surgical excision if > 0.5—1cm
Cyst of canal of Nuck
- Benign painful or painless swelling in the inguinal region and sometimes to the labia majora. A developmental disorder; normally, the canal of Nuck is obliterated in the first year of life.
- Corresponds to encysted hydrocele in males. Cystic dilation can extend from the labia majora to the inernal inguinal ring.
- Treatment is by surgical excision.
Endometriosis
- Presence of normal endometrial mucosa (glands and stroma) abnormally implanted in locations other than the uterine cavity.
- Commoner on episiotomy site, healed laceration scar, site of Bartholin’s surgery.
- Present with vulva pain, dyspareunia, enlarging mass painful during menstruation.
- Treatment is complete surgical removal of affected areas or by laser vaporization.
Other types of cysts include epidermal inclusion cyst and clitoridal cyst.
Benign tumors
Urethral mucosa prolapse
- Complete evagination of mucosa through external meatus.
- Common between 3—11 years, mostly seen in girls under 5 years.
- Presents as bloody stain on underwear or dysuria.
- Treatment
- Medical: analgesic, sitz bath, topical estrogen cream, amoxicillin and flagyl. Most resolve in 2 weeks and recurrence is not common.
- Surgical:
- Excision- catheterize post-op under GA.
- Ligation around a Foley catheter.
- Cryotherapy
- Electrocautery
Urethral caruncle
- Small fleshy outgrowth of the distal edge of urethral mucosa.
- Ectropion off posterior urethral wall.
- Commoner in postmenopausal women.
- Present with post-menopausal vaginal bleeding, dysuria, frequency.
- Treatment
- No treatment necessary if asymptomatic
- Cryosurgery
- Laser therapy
- Excision
Fibromata
- Treatment is excision.
Lipomata
- Treatment is surgical excision.
Hidradenomata
- Sweat gland tumor.
- Usually found in in labia majora and perineum.
- Treatment is by excision.
Hemangiomata
Nevi
Verrucous lesions- rare, usually occurs in the mouth and occasionally on the genitals or feet. Typically develops at sites of chronic irritation and inflammation. Often seen in people who smoke, chew tobacco or drink a lot of alcohol.
Pappilomata- small wartlike growth on the skin or mucus membrane caused by HPV.
Molluscum contagiosum- caused by poxvirus. Produces painless benign raised lesions.
von Recklihausen’s disease- Neurofibromatosis type 1.
Consider pregnancy in all women of childbearing potential.
Do a risk/benefit evaluation.
Minimize prescribing- use ‘tried and tested’ drugs in preference to new agents.
Use the smallest effective dose.
Remember the fetus is most sensitive in the first trimester.
Discuss the potential risks of taking or withholding therapy with the patient.
Seek guidance on the use of drugs in pregnancy- seniors, formulary.
Common presenting complain.
Can be physiological or pathological.
Normal vaginal discharge is a transudate from cervical mucus, secretion from Skene’s and Bartholin’s glands. It is highly acidic due to lactic acid from lactobacilli. It is colorless, odorless, not excessive and not associated with pruritus.
Common etiologies
Prepubertal: poor hygiene, foreign body, non-specific vulvo-vaginitis.
Reproductive age women: infections.
Post-menopausal: low glycogen, estrogen and acidity.
History
Pain, itching.
Color, odor, appearance of vaginal discharge.
Previous episodes
Duration
Use of feminine hygienic products e.g. perfumes, soaps, douching.
Drugs e.g. OCP, antibiotics.
Diabetes mellitus
Non-absorbent tights
Previous treatments
Sexual history
Examination
Inspection- excoriation (chronic skin picking or dermatillomania), etc.
Speculum examination: samples for both sidelab and culture.
Put a drop each on two gas slides.
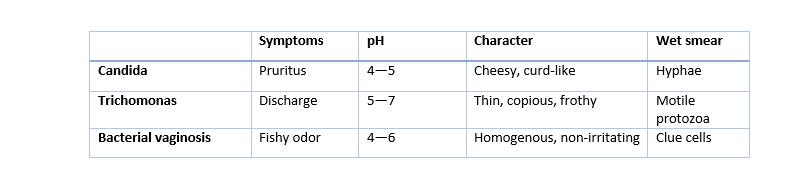
Slide 1:
Add a drop of N/S, put a cover slip. Examine under low power of microscope.
Motile trichomonads- trichomoniasis.
Hyphae of candida.
Clue cells- epithelial cells with microbes attached, for bacterial vaginosis.
Slide 2:
Add a drop of 10% KOH.
Fishy odor confirm bacteria vaginosis i.e. Sniff Test or Whiff Test.
Repeat microscopy: hyphae of candida are easier to see because KOH digest WBC and epithelial cells.
Common causes
Vaginal candidiasis
Mainly caused by C. albican.
Risk factors include DM, HIV, pregnancy, prolonged drug use e.g. antibiotics, OCP, steroids, chronic debilitation.
Presents with intense pruritus with cheesy, curdlike discharge, erythema and burning sensation. Whitish plaques adherent to the vaginal wall with excoriation of vulva skin.
Treatment
- Control underlying disease.
- Discontinue antibiotics
- Avoid douching, non-absorbent underwear
- Drugs: topical antifungal
- Clotrimazole pessary 500mg nocte × 1/52
- Fluconazole 150mg p.o. stat
- Itraconazole 200mg p.o. bd × 1/7
- Ketoconazole 200mg p.o. bd × 5/7 In pregnancy: Nystatin pessary nocte × 1/52
Trichomonal infections
Caused by trichomonal vaginalis- a flagellated protozoa.
Usually sexually transmitted.
Itchy burning sensation, dyspareunia, frothy vaginal discharge which may be white, green or brownish; frothy due to gaseous fermentation by a commensal aerogenic streptococcus. Vulva edema, less erythema than candida. pH 5—6.
Treatment is with metronidazole for both partners.
Bacteria vaginosis
Overgrowth of bacteria: Gardrenella vaginalis, anerobes (Mobilincus sp, Bacteroides), and Mycoplaspla hominis.
Risk factors: sexually active, IUCD, low socioeconomic status, previous STD.
Profuse, thin, homogenous grey/white/yellow malodorous discharge, fishy smell due to amines. Minimal or no pruritus, pH > 7.0.
Risk factor in post abortal sepsis, preterm delivery, SPROM, chorioamnionitis, postpartum endometritis.
Treatment
- Metronidazole p.o. 500 mg bd x 1/52 or 2gm stat.
- Clindamycin cream 5g PV nocte x 1/52.
- Clindamycin 300 mg bd x 1/52.
- In pregnancy:
- Metronidazole 250 mg tds x 1/52 or metronidazole 2gm stat.
- Clindamycin 300 mg bd x 1/52.
Gonococcal infection
Due to Neisseria gonorrhea.
Painful vulva swelling, dysuria, purulent discharge 2—7 days or longer after coitus with infected partner.
Intracellular diplococcic on microscopy.
Culture on Thayer-Martin plate, transfer swabs in Stuart’s transport medium.
Treatment is with procaine penicillin, ampicillin, augmentin, or erythromycin.
Other causes
Post-menopause:
- Mainly due to atrophic vaginitis. Rule out cancer via EUA, then give topical steroids.
Prepubertal:
- Poor hygiene, estrogen lack, non-specific vulvovaginitis.
- Rule out sexual abuse in specific vulvovaginitis.
- Parasites such as pinworm, threadworm.
- Emphasize perineal hygiene.
Genital warts
A benign lesion of vulva and vagina.
Also called condyloma acuminatum
Caused by Human Papilloma Virus infection- e.g. Subtypes 6 and 11.
Appear as popular swelling mainly on the labia and posterior part of the introitus. May also affect the lower and middle third of the vagina and the cervix.
Complications: ulceration, secondary infection, hemorrhage, malignant transformation, transmission to the neonate causing laryngeal papilloma.
Treatment include cryotherapy, electrocautery (diathemy), trichloroacetic acid, podophyllin, podophyllotoxin. Note that the last 2 are contraindicated in pregnancy.
Active genital herpes is an indication for Caesarean
Female genital mutilation (FGM) or female genital cutting/circumcision.
It is the total or partial removal of the female external genitalia for non-medical reasons.
Practiced by people of all faith and social status. It is especially prevalent in 28 African countries, Middle East and Asia. Now seen in Europe, USA and Australia due to migration.
About 138 million affected and about 2 milion at risk annually.
Usually performed by herbalists, traditional birth attendants (TBA) or local circumcisers without anesthesia with physical restraint; they then rub herbs on it. Health workers usually from endemic areas occasionally do it from ‘pity’.
WHO has declared FGM illegal and a violation of human right. In addition, it is an offence for medical personnel to practice FGM
Reasons for FGM
To ensure virginity.
To control female sexuality.
Hygiene and cleanliness.
Some believe the baby’s head must not touch the clitoris during delivery.
Some also believe that a narrow opening heightens male sexual pleasure and fertility.
As a traditional/cultural practice/religious obligation.
Timing depend on the culture, but it can be done in
- Infancy
- Early childhood
- Teenage years
- During preparation for marriage
It is a mark of social acceptance and guarantee for marriage in some culture. Many parents approve of it and there may be a ceremony and gift preparation.
Classification
Type 1: excision of the prepuce with/without parts or all of the clitoris.
Type 2: excision of the clitoris with partial or total excision of the labia minora.
Type 3: excision of part or all of the external genitalia and stitching/narrowing of the vagina opening (infibulation).
Type 4: unclassified- includes applying corrosive substances for narrowing the vagina, pricking, piercing, incising, stretching, scraping or other harmful procedures performed on the clitoris and or the labia.
Complications
Short term
Hemorrhage
Pain
Urinary retention
Secondary infection
Transmission of infection- HIV, Hepatitis
Anemia
Death
Long term
Keloid, clitoral cyst
Sexual dysfunction
Recurrent UTI
Renal failure
Acquired gynetresia with hematocolpos
Obstructed labor
Psychological disorders
Prevention
Health education.
Dialogue with cultural, religious and traditional leaders.
Legislation.
Replacement with healthy social alternatives for initiation into adulthood.
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions