What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
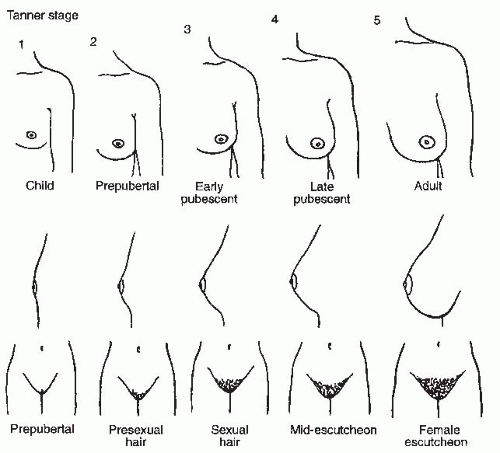
Definition: failure of the development of any secondary sexual characteristic by the age of 14 years.
In the presence of secondary sexual characteristics, menstruation ought to occur within 2 years of the establishment of this development.
Hence, primary amenorrhea is defined as a failure of spontaneous menstruation by the age of 16 years in the presence of normal secondary sexual characeristics, or 14 years in the absence of secondary sexual characteristics.
There are five changes that occur, known as the secondary sexual characteristics.
In girls these are
- Breast
- Pubic hair
- Axillary hair development,
- The growth spurt, and the
- Onset of menstruation
.jpg)
.jpg)
Basic requirements for normal menstrual function
- Genital outflow tract
- Uterus
- Ovary
- Anterior pituitary
- Hypothalamus or CNS
Causes of primary amenorrhea
- Imperforate Hymen
- Transverse Vaginal Septum
- Absent vagina and functioning uterus
- XY Female
- Androgen Insensitivity Syndrome
- Gonadal agenesis
- Turner's syndrome
- Resistant ovary syndrome
- Constitutional delay
- Kallman syndrome
- Other causes
Imperforate Hymen
May present at two ages of development. Early childhood when the infant presents with a bulging hymen and mucocele. It may also present in later life when a pubertal girl complains of intermittent abdominal pain, which is usually cyclical.
The pain is due to dysmenorrhea associated with the accumulation of menstrual blood within the vagina known as hematocolpos. It is also known as cryptomenorrhea.
When some blood accumulates within the uterine cavity, it is called hematometra. As the mass enlarges there may be associated difficulty with micturition and defecation.
Examination will reveal an abdominal swelling and a tense bulging bluish membrane which is the hymen.
It results from an error in urogenital sinus canalization
Treatment is hymenectomy/cruciate incision.
.png)
.jpg)
.jpg)
Transverse Vaginal Septum
These girls present with cyclical abdominal pain due to the development of a hematocolpos
Clinical appearance is very different from that of an imperforate hymen.
An abdominal mass may be palpable but inspection of the vagina shows that it is blind ending.
The bulging is pink not blue.
Rectal exam may reveal a mass.
The hymenal remnants are often seen separately. Transverse vaginal septum may occur at three levels, known as a lower, middle or upper third septum.
This results from failure of fusion of the Mullerian duct and urogenital sinus derived portion of the vagina.
Treatment is with a cruciate incision.
Absent vagina and the functioning uterus
This is a rare phenomenon when embryologically the uterine body has developed normally, but there is failure of development of the cervix.
This leads to failure of the development of the upper vagina.
The presenting symptom is again cyclical abdominal pain but there is no pelvic mass because there is no vagina.
Although a small haematometra may be present, retrograde menstruation occurs leading to the development of endometriosis and in some patients, pelvic adhesions.
This is known as the Mayer-Rokitansky-Kuster- Hauser syndrome (or the MRKH syndrome). It is also known as Mullerian dysgenesis or utero-vaginal agenesis. In this condition, there is failure of development of the Mullerian ducts. It is usually associated with other skeletal and urogenital malformations but it can also be isolated.
This is the second most common cause of primary amenorrhea second only to Turner syndrome.
The individuals are genetically female with 46XX karyotype.
Secondary sexual characteristics are normal as would be expected as ovarian function is unaffected.
Examination of the genital area discloses normal female external genitalia but with a blind ending vaginal dimple which is usually not more than 1.5 cm in depth.
The uterine development is usually very rudimentary, often small uterine remnants (anlage) are found on the lateral pelvic side walls.
40% of these patients have renal anomalies and recognizable skeletal abnormalities.
.jpg)
XY Female
Individual may have an XY karyotype and a female phenotype. This may be due to
- Failure of testicular development
- Enzymatic failure of the testis to produce androgen particularly testosterone
- Androgenic receptor absence or failure of function
Androgen Insensitivity Syndrome
There is a structural abnormality with the androgen receptor, due to abnormalities of the androgen receptor gene, which results in a non-functional receptor.
The masculinizing effect of testosterone during normal development is absent.
It can be partial or complete depending on the amount of residual androgen receptors. In complete AIS, the individual develop female external genitalia with normal labia, clitoris and vaginal introitus, but the vagina ends blindly and they lack uterus and fallopian tubes.
All the Mullerian-derived structures are absent because the developed gonads are morphologically testes and the Sertolli cells produce anti-Mullerian hormones which inhibit Mullerian development
Patients are phenotypically female with normal breast development. At puberty, the increasing levels of androgens are converted to estrogens with normal female breast development and distribution of body fat.
Pubic hair is very scanty in these patients as there is no androgen response in target tissues.
The vulva is normal and the vagina is usually short.
The uterus and tubes are absent in this particular version of the XY female.
The testes are usually found in the lower abdomen, but occasionally may be found in hernial sacs in childhood.
Gonadal agenesis
46XX:
The 46XX pure gonadal dysgenesis is an autosomal recessive disorder and other genes other than those located on the X chromosome are involved.
46XY OR 45X/46XY:
In 46XY or 45X/46XY, absence of testicular determining factor or its receptor are postulated as the cause of the failure of differentiation of the gonad
There is absence of testicular development.
Turner's syndrome
In Turner's syndrome ovarian development is normal until 20 weeks' of gestation and at this stage oocytes are found in the ovaries.
Further maturation is impaired and a massive atresia occurs during the latter part of pregnancy.
The ovaries in most individuals consist solely of stroma and are unable to produce estrogen.
There is a normal female phenotype and internal genital development is also normal.
The loss of an X chromosome results in short stature.
.jpg)
Resistant ovary syndrome
There are elevated levels of gonadotropins in the presence of apparently normal ovarian tissue.
Patients do have some degree of secondary sexual characteristic development but never produce adequate amounts of estrogen to result in menstruation.
Constitutional delay
Normal secondary sexual characteristics exist. There is no anatomical anomaly and endocrine investigations are all normal.
Kallman syndrome
The olfactogenital syndrome.
There is isolated GnRH deficiency.
There is a hypogonadotrophic state.
The pituitary gland is normal and stimulation with exogenous GnRH leads to normal release of gonadotrophins.
This condition arises due to a maldevelopment of neurones in the arcuate nucleus of the hypothalamus. These neurones are derived embryologically from the olfactory bulb, and therefore some patients may be unable to smell (anosmia).
They are of normal height.
Other causes
Anorexia nervosa/Weight loss
Excessive exercise
Hyperprolactinemia .These cause more of secondary amenorrhea
Ovarian failure - from chemotherapy and radiotherapy for childhood malignancies.
Galactosaemia - deficiency of galactose-1- phosphate uridyl transferase. The galactose metabolites may induce ovarian failure.
Heterosexual development
- Congenital adrenal hyperplasia
- Androgen secreting tumors of the ovary
- 5 alpha reductase deficiency
- Absent Mullerian inhibitor
- True hermaphrodite
- Partial androgen receptor deficiency
.jpg)
.jpg)
Management
Examine secondary sexual characteristics and Height
In the presence of normal secondary sexual characteristics, outflow tract obstruction should be excluded.
Pelvic ultrasound
Magnetic resonance imaging (MRI) or computed tomography (CT) scanning.
Karyotype.
Gonadotrophin and prolactin levels
In girls with absent uterus, vaginoplasty may be considered at the appropriate time
Use of vaginal dilators
In XY females, remove gonads because of the risk of malignancy
Counselling and sharing of information on karyotype should be done appropriatey, not too early.
In outflow tract obstruction, cruciate incision/reconstructive surgery should be considered.
In constitutional delay, review annually and consider a cycle of combined pills.
Hormone replacement therapy in hypogonadotrophic hypogonadism to induce 2° sexual characteristics Treatment is over 3-5 yrs
Estrogen for 2yrs then 2-3yrs of gradual introduction of progesterone.
Isolated GnRH deficiency hormone
Replacement therapy will need to be instituted to induce secondary sexual characteristic development.
These patients can be informed that they are infertile and that ovulation induction in the future can be invoked using various fertility regimes.
Cessation of menstruation for 6 consecutive months in a woman who has previously had regular periods, is the usual criteria for investigation.
Cessation for 3 cycles in oligomenorrheic women
Women with secondary amenorrhea must have
- A patent lower genital tract,
- An endometrium that is responsive to ovarian hormone stimulation and
- Ovaries that have responded to pituitary gonadotrophins.
Causes of Secondary Amenorrhea
- Asherman's Syndrome
- Polycystic ovarian disease
- Premature ovarian failure
- Hyperprolactinemia
- 2° hypogonadotrophic hypogonadism
- Gonadal dysfunction
- Weight related amenorrhea
- Others
Asherman's Syndrome
Intrauterine adhesions prevent normal growth of the endometrium. It is also known as uterine synechae.
This may be the result of a too vigorous endometrial curettage affecting the basalis layer of the endometrium or adhesions
May follow an episode of endometritis.
It may be possible to induce a withdrawal bleed using a combined estrogen/progestagen preparation.
Intrauterine adhesions may be seen on a hysterosalpingogram (HSG)
The diagnosis is usually suspected following negative response from progestogen challenge or the presence of multiple filling defects or total occlusion of endometrial cavity on hysterosalpingography.
Hysteroscopic inspection of the uterine cavity will confirm the diagnosis and enable treatment by adhesiolysis.
A 3-month course of cyclical progesterone/estrogen should be given.
Insert Foley’s catheter for 7 days or a non-copper intrauterine contraceptive device such as Lippes loop for 2-3 months into the uterine cavity to prevent recurrence of adhesions and allow endometrial development to occur.
Cervical stenosis may rarely follow cone biopsy
The treatment is cervical dilatation
Polycystic ovarian disease
The polycystic ovary syndrome is a heterogeneous condition which is defined by the presence of two out of the following three criteria
- Oligo- and/or anovulation
- Hyperandrogenism (clinical and/or biochemical)
- Polycystic ovaries, with the exclusion of other etiologies.
PCOS therefore encompasses symptoms of menstrual cycle disturbance and as such is the commonest cause of secondary amenorrhea.
The pathophysiology of the PCOS appears to be multifactorial and polygenic.
Key features include
- Menstrual cycle disturbance,
- Hyperandrogenism and
- Polycystic ovaries.
An ovary with 12 or more follicles measuring 2-9 mm in diameter and increased ovarian volume (>10 cm3) on transvaginal ultrasound.
The PCOS is familial and various aspects of the syndrome may be differentially inherited.
Investigations-
Hormonal assays
hCG to rule out pregnancy, the most common cause of secondary amenorrhea.
High FSH suggest primary ovarian failure, a high LH or raised LH to FSH ratio suggests PCOS.
A raised testosterone can indicate PCOS, AIS, or CAH but usually, it indicate PCOS.
Treatment
Weight control
Use of insulin sensitizers
Ovulation induction using clomiphene citrate with tamoxifen or cyclofenil, gonadotropins (FSH).
Ovarian drilling
Cyclical combined oral contraceptive pills or cyclical progestin every 3 months if pregnancy is not desired.
Treatment of other associated disorders
Premature ovarian failure
By definition is the cessation of periods accompanied by raised gonadotropin level prior to the age of 40 years.
It may occur at any age.
It is due to chromosomal abnormalities in 2-5% of women.
The most common cause is autoimmune disease.
Others are infection, previous surgery, chemo- and radiotherapy.
Hyperprolactinemia
It is the commonest pituitary cause of amenorrhea.
May result from a prolactin-secreting pituitary adenoma, or from a non-functioning 'disconnection' tumor in the region of the hypothalamus or pituitary, which disrupts the inhibitory influence of dopamine on prolactin secretion.
Mechanism of hyperprolactinemia and amenorrhea is probably due to the inhibitory effects of raised prolactin on the pulsatile release of GnRH from the hypothalamus thereby blocking the LH surge neede for ovulation and also interfering with the actions of gonadotropins on the ovary itself.
Hypothyroidism, polycystic ovary syndrome and drugs e.g. the dopaminergic antagonist phenothiazines, domperidone and metoclopramide.
Patients may present with galactorrhea and visual field defects.
Investigations- Prolactin assay, lateral skull Xray, CT scan, MRI. Often microadenomas might not appear in initial scans and follow-up scans are required to identify tumors that develop in size later.
Treatment- dopamine agonists (bromocriptine, cabergoline), transphenoidal adenectomy, radiotherapy and hormone replacement
2° hypogonadotrophic hypogonadism
Sheehan's syndrome- the result of profound and prolonged hypotension on the sensitive pituitary gland, enlarged by pregnancy, following a major obstetric hemorrhage.
Systemic conditions- sarcoidosis, tuberculosis
Head injury
Cranial irradiation
Pituitary Function should be assessed and the appropriate replacement should be instituted.
Gonadal dysfunction
Leading to amenorrhea
May follow
- Renal failure
- Liver disease
- Endocrinopathies - thyrotoxicosis, Cushing’s syndrome
- Autoimmune dx
- Diabetes mellitus
Weight related amenorrhea
Weight can have profound effects on gonadotropin regulation and release.
Weight and eating disorders are common in women. A regular menstrual cycle will not occur if the BMI is less than 19 kg/m2.
Fat appears to be critical to a normally functioning hypothalamic-pituitary gonadal axis.
It is estimated that at least 22% of body weight should be fat to maintain ovulatory cycles.
This is required for extra ovarian aromatization of androgens to estrogens.
To cause amenorrhea the loss must be 10-15% of the women's normal weight for height.
Others
Anorexia nervosa
Stress
Exercise related amenorrhoea
Iatrogenic- radiation to the abdomen/pelvis or chemotherapy.
- Gynaecological procedures such as oophorectomy, hysterectomy and endometrial resection
Acquired gynetresia- occlusion of vaginal lumen following insertion of corrosive herbs into the vagina or prolonged obstructed labor. Signs and symptoms similar to imperforate hymen.
The treatment depends on identified cause of amenorrhea.
Determine the cause and the level of malfunction on the hypothalamo-pituitary- ovarian- endometrial axis
Investigate to confirm diagnosis and follow up
Assess other associated problems such as infertility i.e. the desire for pregnancy
Progesterone challenge- this test indirectly determines whether the ovary is producing estrogen. The test depends on the fact that progesterone will be unable to provoke bleeding in the absence of circulating estrogen necessary for priming the endometrium. Medroxyprogesterone or progesterone can be used. No bleeding suggests there is low estrogen or outflow tract abnormality such as Asherman’s syndrome.
Estrogen-progesterone challenge- if progesterone challenge test is negative, this might help distinguish between hypoestrogenism and outflow tract obstruction. Estrogen is given for endometrial proliferation followed by a progestin to induce withdrawal bleeding. Bleeding suggest hypoestrogenic state, while absence of bleeding may be due to Asherman’s syndrome or cervical stenosis.
Hysterosalpingography or hysteroscopy can be carried out to make a diagnosis of Asherman’s syndrome or other outflow tract abnoralities.
Ovulation induction with clomiphene citrate, letrozole, FSH, human menopausal gonadotropin (hMG), human chorionic gonadotropin, metformin, or laparoscopic ovarian drlling.
Hormone replacement
Multidisciplinary management
Osteoporosis- patients with amenorrhea associated with low estrogen levels are at increased risk of osteoporosis.
Cardiovascular disease
Endometrial hyperplasia
Endometrial carcinoma
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions