What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
- Definitions of diarrhea include:
- Increases in volume or fluidity of stools
- Changes in consistency, and increased frequency of defecation
- One of the leading causes of morbidity and mortality
- A child may have more than 3 episodes in a year
- The major cause of death (80%) is dehydration—resulting from fluid and electrolyte loss in stools
- It is an important cause of malnutrition due to reduced intake, increased loss, and increased requirements
- Route of transmission
- Fecal-oral route – ingestion of contaminated water, food, and direct contact with feces
- Poor hygiene and food handling
- Allowing an infant to crawl around and play where human or animal fecal material is present
- Risk factors that predispose to diarrhea
- Lack of exclusive breastfeeding for 4-6 months
- Use of infant feeding bottles
- Drinking water contaminated with feces
- Failing to wash hands after defecation
- Poor fecal disposal
- Host factors
- Lack of exclusive breastfeeding
- Malnutrition
- Immunodeficiency or suppression
- Age – common in the first 2 years (6-11 months) due to decreasing maternal antibodies, lack of active immunity, and introduction of contaminated food
- Season
- Peaks
- Bacterial infections occur more in the warm season
- Viral diarrhea occurs more in winter
- Viral diarrhea occurs throughout the year in the tropics
- Acute diarrhea: lasts a few days
- Persistent diarrhea: lasts at least 14 days
- Chronic diarrhea: lasts more than 4 weeks and is due to a chronic illness
- Dysentery: diarrhea with visible blood in stool
- Toddler’s diarrhea: recurrent episodes of mild to moderate diarrhea of variable duration in toddlers, with no identifiable cause and no associated constitutional symptoms
- Traveler’s diarrhea: caused by pathogenic organisms in contaminated food
Diarrhea can result from various pathophysiologic mechanisms affecting the gastrointestinal tract. The following are key mechanisms that lead to diarrhea:
Stimulation of Intestinal Secretions:
- Secretory Diarrhea: Caused by toxins that stimulate the secretion of electrolytes and water into the intestinal lumen without damage to the mucosa.
- Examples: Vibrio cholerae (cholera), Enterotoxigenic E. coli (ETEC)
Mucosal Damage:
- By Adherence: Pathogens attach to the intestinal mucosa, leading to impaired absorption and diarrhea.
- Examples: Enteroadherent E. coli, Giardia lamblia, Cryptosporidium
- By Invasion: Pathogens invade and damage the intestinal mucosa, leading to inflammatory diarrhea.
- Examples: Shigella, Enteroinvasive E. coli (EIEC), Campylobacter, Salmonella
Increased Osmolality of Intestinal Luminal Content:
- Osmotic Diarrhea: Occurs when non-absorbable substances in the intestinal lumen draw water into the bowel, increasing stool volume.
- Examples: Malabsorption syndromes, ingestion of osmotic agents
Abnormal Intestinal Motility:
Abnormalities in the motility of the intestines can lead to either rapid transit, reducing absorption, or slow transit, promoting bacterial overgrowth and diarrhea.
Ion Transport Defect:
Defects in the transport of ions across the intestinal epithelium can lead to either reduced absorption or increased secretion of fluids, resulting in diarrhea.
These mechanisms often overlap and contribute to the clinical presentation of various diarrheal diseases.
- Virus:
- Rotavirus
- Bacteria:
- Enterotoxigenic E. coli (ETEC)
- Shigella
- Campylobacter jejuni
- Protozoa:
- Cryptosporidium
- Yersinia enterocolitica
Organisms that Invade Mucosa
- Shigella
- Enteroinvasive E. coli (EIEC)
- Campylobacter jejuni
- Salmonella
- Entamoeba histolytica
Other Conditions Causing or Associated with Diarrhea
- Diseases associated with diarrhea:
- Malaria
- Measles
- Acute Respiratory Infections (ARI)
- Drugs
- Diarrhea: sudden onset, typically subsides in 3-5 days
- Vomiting: common
- Prodromal illness: may suggest viral etiology
- Fever: no diagnostic significance
- Abdominal pain, blood, mucus: possible invasive agent
- Signs: dehydration, malnutrition
Assessment of Dehydration
Look for any high-risk factors:
- Infants
- Discontinuation of breastfeeding
- Frequent stooling (>8 stools/day)
- Severe malnutrition
Use recent weight loss as a percentage of total body weight if records are available, or assess the presence and severity of dehydration based on clinical signs.
| Clinical Signs of Dehydration | ||||
|---|---|---|---|---|
| None | Mild | Moderate | Severe | |
| General Appearance* | Well, Alert | Alert | Restless, Irritable | Lethargic, Drowsy or Unconscious |
| Eyes | Normal | Normal | Sunken | Grossly Sunken |
| Tears* | Present | Present | Reduced | Absent |
| Anterior Fontanelle | Normal | Normal | Depressed | Sunken |
| Mucous Membrane* | Moist | Moist | Dry | Very Dry |
| Thirst* | Normal | Thirsty | Thirsty, Drinks Eagerly | Drinks Poorly or Unable to Drink |
| Skin Turgor | Normal | Normal | Returns Slowly (≥2s) | Returns Very Slowly (or Tenting >2s) |
| Capillary Refill* (Perfusion) + Extremities | Normal | Normal | Delayed (2-4s) | Delayed ++ (>4s) + Cold Limbs |
| Pulse Volume | Normal | Normal | Weak | Feeble or Impalpable |
| Pulse Rate | Normal | Normal | Increased | Increased |
| Blood Pressure | Normal | Normal | Normal or Decreased | Decreased or Unrecordable |
| Respiration | Normal | Normal | Increased | Rapid & Deep |
| Urine Output | Normal | Normal | Decreased | Decreased or Absent |
| Percentage Deficit | <3% | 3-5% | 6-9% | 10% or more |
High Risk Factors for Dehydration in a Child with Diarrhea
- Age below 12 months
- Discontinuation of breastfeeding
- Frequent stools (>8/day)
- Vomiting ++
- Severe malnutrition
Oliguria:
- Acute Renal Failure: Severe dehydration and fluid loss from diarrhea can lead to decreased kidney perfusion and acute renal failure.
Electrolyte Imbalance:
- Decreased Potassium (Hypokalemia): Due to loss of potassium in stool.
- Decreased Bicarbonate (Hypobicarbonatemia): Resulting from loss of bicarbonate and metabolic acidosis.
- Hypo- or Hypernatremia: Imbalances in sodium levels can occur due to fluid loss or replacement therapy.
Lactose Intolerance:
- Secondary Lactose Intolerance: Temporary or persistent lactose intolerance may develop due to damage to the intestinal mucosa, affecting lactase enzyme production.
Malnutrition:
- Chronic or severe diarrhea: Can lead to poor absorption of nutrients and subsequent malnutrition.
Death:
In severe cases, complications from dehydration, electrolyte imbalance, and malnutrition can be life-threatening, particularly in vulnerable populations like young children and the elderly.
- Electrolyte & Urea: To assess electrolyte imbalances and kidney function.
- Full Blood Count (FBC) / Microscopy, Culture, and Sensitivity (M/C/S): To evaluate for infection and identify potential pathogens.
- Blood Culture: To detect bacteremia or septicemia in severe cases.
- Blood Gas Analysis: For assessing acid-base status, especially in severe cases or if clinically acidotic.
- Stool Examination:
- Microscopy, Culture, and Sensitivity (M/C/S): To identify pathogens and determine appropriate treatment.
- Reducing Substances: To check for malabsorption, such as in carbohydrate malabsorption syndromes.
- Urine Culture: To rule out urinary tract infections, which can sometimes present with symptoms similar to gastrointestinal infections.
- Prevent dehydration
- Correct dehydration
- Maintain or improve nutrition
- Treat aetiological agents if any
Prevention of Dehydration
- Advise unrestricted oral fluids
- Continue breastfeeding
- Prescribe 10ml/kg of ORS after each watery stool passed
- Zn 10-20mg/day
- Educate mother: personal hygiene, immunization, homemade SSS
Correction of Dehydration
Note:
- Rehydration can be achieved either:
- Orally (ORT)
- Intravenous route
- ORT is used for most cases
- Rehydration (correction of deficit) is achieved in 4-6 hours.
| Standard ORS Solutions | ||
|---|---|---|
| New | Old | |
| Na* | 75 mmol/L (2.6 g/L) | 90 mmol/L (3.5 g/L) |
| Cl* | 65 mmol/L (1.5 g/L) | 80 mmol/L (2.5 g/L) |
| K | 20 mmol/L (1.5 g/L) | 20 mmol/L (1.5 g/L) |
| Glucose* (anhydrous) | 75 mmol/L (13.5 g/L) | 111 mmol/L (20 g/L) |
| TriNa Citrate | 10 mmol/L (2.9 g/L) | 10 mmol/L (2.9 g/L) |
| Osmolality* | 245 | 310 |
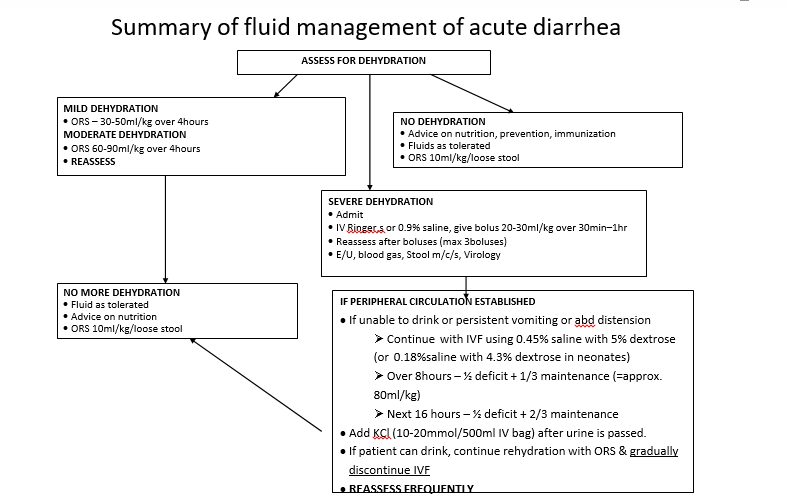
REHYDRATION
Mild Dehydration
- 30-50 ml/kg of ORS over 4 hours
Moderate Dehydration
- 60-90 ml/kg of ORS over 4 hours
Re-assess after 4 hours
ORT is Inappropriate for
- Initial treatment of severe dehydration with signs of shock
- Patients with paralytic ileus or marked abdominal distention
- Patients unable to drink (However, ORS solution can be given to such patients through an N/G tube if IV is not possible)
Intravenous Therapy (IVT)
- Mainly used for initial treatment of severe (life-threatening) dehydration, to rapidly restore blood volume and correct shock.
- In severe dehydration with shock:
- Give 20-30 ml/kg IV boluses of Ringer’s lactate or normal saline until organ perfusion is restored. Then continue rehydration with ORT.
- If the child is not able to drink:
- Continue rehydration with IVT using 0.45% saline in 5% dextrose (or 0.18% saline in 4.3% dextrose based on serum sodium values).
- Calculate deficit and maintenance.
- Give ½ deficit and ⅓ maintenance in 8 hours and the remaining deficit and maintenance in 16 hours.
- Add KCL (10-20 mmol/500 ml bag) as soon as urine is passed.
Maintenance Therapy
- Maintenance Phase to prevent recurrence of dehydration.
- This should be given orally as ORS or other fluids if the child can drink.
| Maintenance Fluid Requirement | |
|---|---|
| Body Weight (kg) | Maintenance Fluid Requirement |
| ≤ 10 | 100 ml/kg/day |
| 11-20 | 1000 ml plus 50 ml/kg for each kg above 10 kg |
| > 20 | 1500 ml plus 20 ml/kg for each kg above 20 kg |
Role of Drugs in the Treatment of Acute Diarrhea
- Antidiarrheal, antiemetic, or antisecretory agents are of no benefit and some can be dangerous.
- Antimicrobials are only indicated in:
- Severe Shigella infection
- Moderate to severe Clostridium infection associated with colitis
- Enteroinvasive E. coli infection
- Salmonella enteritis in the very young, immune-compromised, or systemically ill child
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Contributors
Jane Smith
She is not a real contributor.
John Doe
He is not a real contributor.
Send your comments, corrections, explanations/clarifications and requests/suggestions