What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
- Tertiary
- Training
- Service
- Research
- Secondary
- Service
- Training
- Research
- Primary
- Service
- Outreaches
- Community data source
Tertiary – federal government
- Teaching hospitals
- Federal medical centres
- National orthopaedic hospitals
- National psychiatric hospitals
Secondary – state governments
- General hospitals
- State hospitals
Primary
- Comprehensive health centres
- Basic health centres
- People who need health services the most are least provided with the services
- Disparity between developed and developing world
- Disparity between urban and rural in the developing world
- Equity and social justice
- Alma ata declaration 1978: It emerged as a major milestone of the twentieth century in the field of public health, and identified primary health care as the key to attainment of the goal of Health for All. Specifically, the declaration outlined eight essenntial components of PHC.
Nigeria since independence in 1960 has adopted five national health plans, the first four being incorporated into the various plans:
- 1st: 1962 – 68
- 2nd: 1970 – 74
- 3rd: 1975 – 80
- 4th: 1981— 85
- 5th: 1987— 91
National Health Policy and strategy to Achieve primary health care was formulated in 1988
The 1988 Medical Health Policy adopted Primary Health Care as the key to attaining Health for All (Alma Ata). The key elements of the policy were:
- Education on Prevailing health problems and ways to prevent them;
- Promotion of food Supply and proper nutrition;
- Maternal and childcare including family planning;
- Prevention and control of local endemic diseases;
- Provision of essential Drugs and supplies
- Immunization against childhood diseases
- Provision of safe water and Environmental Sanitation
The establishment of National Primary Health Care Development Agency (NPHCDA), through legislation by the Federal Government
1985 was then the beginning of the “Kuti Years” which will be remembered by the increased budgetary allocation to Health Sector and the creation of public awareness for PHC.
Primary health care is essential care based on practical, scientifically sound, socially acceptable methods and technology, made universally accessible to individuals and families in the community through their full participation and at a cost that the community and country can afford to maintain at every stage of its development in a spirit of self-reliance and self-determination.
Emphasis
- Scientifically sound
- Appropriate technology
- Affordable
- Community participation
- Sustainable in approach
- Country/community ownership
- Community based
- Working place
- Living place
Minimum
- Health education concerning prevailing health problems and the methods for preventing and controlling them
- Immunisation against vaccine preventable diseases
- Maternal and child health care, including family planning
- Appropriate treatment of common diseases and injuries
- Promotion of food and proper nutrition
- Environmental sanitation and adequate supply of safe water
- Essential drug supply
- Prevention and control of locally endemic diseases
.png)
Optional
- Community mental health
- Oral and dental health
- Appropriate record keeping
- Community participation
- Appropriate technology
- Affordable/cost effective
- Accessible
- Culturally acceptable
- Scientifically sound
- Intersectoral collaboration
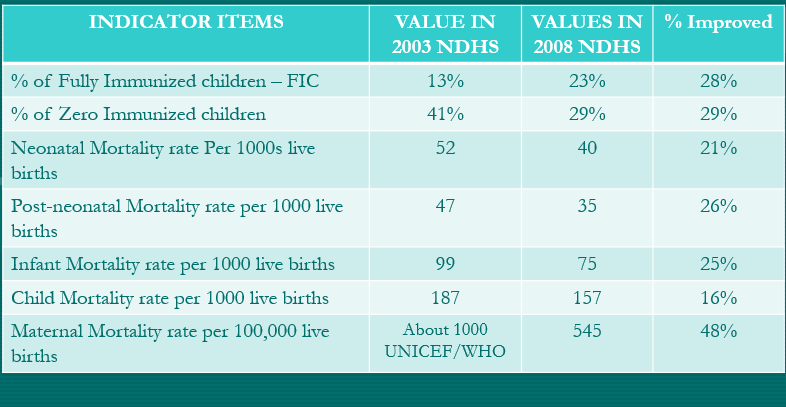
Comparison of Values of Selected Health Indicators for 2003-2008 NDHS as a Measure of Success of the health Sector Reform
Other Accomplishments
- Progress made towards strengthening primary health care included rehabilitation and re-equipping of 208 existing primary health centers in various parts of Nigeria.
- Over 500 new model primary health centers were constructed and equipped in various parts of Nigeria.
- Progress made towards improving blood safety and safe injection practices included: commissioning of 6 zonal blood centers and also in Abuja.
- Poor service delivery
- Policy gaps, inconsistency and discontinuing in policy and implementation.
- Neglected infrastructures
- Weak and obsolete information management system
- Inadequate health budget
- Poorly remunerated and motivated staff
- Uneven distribution of staff.
- Poor quality of care
- Disease burden still high e.g. hypertension, malaria and RTA
Other problems
- Funding
- Sustenance
- Donor dependency syndrome
- Poor staff commitment
- Poor staff motivation
- Mismanagement of resources
- Lack of intersectoral collaboration
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions