What You Will Learn
After reading this note, you should be able to...
- Recognize the role of preoperative assessment in evaluating health and optimizing care.
- List objectives, including medical evaluation, risk reduction, and anesthesia planning.
- Explain key steps: problem identification, risk assessment, preparation, and building rapport.
- Understand the impact of family history on anesthesia, especially in hereditary conditions.
- Evaluate challenges in anesthesia linked to chronic smoking and alcoholism.
- Recognize potential drug interactions and complications related to specific anesthesia drugs.
- Describe elements of a thorough physical examination during preoperative evaluation.
- Explain the Mallampati Classification system for assessing tracheal intubation difficulty.
- Understand guidelines for preoperative lab investigations based on patient history.
- Utilize the ASA physical status classification to assess surgery and anesthesia risk.
- Understand fasting guidelines for different age groups before surgery.
- Recognize the need for preoperative preparation to optimize physiological variables.
- List essential steps in a preoperative checklist for optimal patient care.
Note Summary
Introduction:
Preoperative assessment is a critical step before surgery, aimed at evaluating patient health, minimizing risks, and planning for optimal perioperative care.
Objectives:
- Evaluate patient's medical condition.
- Optimize health for surgery.
- Minimize anesthesia risks.
- Plan anesthesia and perioperative care.
- Establish rapport and educate the patient.
- Obtain informed consent.
Steps:
-
Problem Identification
- Thorough history: present and past illnesses, lifestyle.
- Special attention: chronic smoking, alcoholism.
- Drug and family history.
-
Physical Examination
- General, respiratory, cardiovascular assessment.
- Airway evaluation using Mallampati classification.
-
Laboratory Investigations
- Urinalysis, Hemoglobin, Electrolytes, Chest X-ray, ECG, Sickle Cell Status, additional tests as needed.
-
Risk Assessment
- Use ASA classification to determine fitness.
- 'E' for emergency procedures.
-
Fasting Guidelines
- Clear fluids: 2 hours, Breast milk: 4 hours, Light meal: 6 hours.
-
Preoperative Preparation
- Further investigations for specific conditions.
- Stabilization with fluids, blood, drugs as needed.
- Checklist: patient identification, surgical site marking, informed consent.
Conclusion:
A systematic approach to preoperative assessment ensures patient safety, optimizes outcomes, and minimizes complications. Thorough history, examination, and tailored preparations are key elements in this process.
closeClick here to read a summary
The preoperative assessment is a medical check-up and laboratory investigations done before surgery:
- To assess the patient’s physical condition and any other medical problems/diseases
- To identify factors that significantly increase the risk of complications, and modify the procedure appropriately
- To identify the appropriate anaesthetic technique to be used
- To ensure safety of perioperative care, optimal resource use, improved outcomes and patient satisfaction
- Several studies have shown that inadequate preoperative preparation of patients may be a major contributory factor to peri-operative catastrophes.
- It is therefore essential that the anaesthetist visits every patient in the ward or the patient is seen in the pre-anaesthetic clinic before surgery to assess fitness for anaesthesia.
- To evaluate the patient’s medical condition
- To optimize the patient’s medical condition for anaesthesia and surgery
- To determine and minimize risk factors for anaesthesia
- To plan anaesthetic technique and perioperative care
- To develop a rapport with the patient in order to reduce anxiety and facilitate the conduct of anaesthesia
- To inform and educate the patient about anaesthesia, perioperative care, and pain management
- To obtain informed consent for anaesthesia
- Problem identification
- Risk assessment/optimization
- Preoperative preparation
- Plan anaesthetic technique
Establishing Rapport
- The anaesthetist discusses possible causes of anxiety regarding anaesthesia and surgery with the patient.
- The anaesthetist explains how the patient will be cared for during the peri-operative period.
- The anaesthetist explains the various techniques of anaesthesia available for the planned surgery.
- The anaesthetist explains to the patient the options and measures for postoperative pain relief.
- The anaesthetist obtains informed consent.
Problem Identification
- History
- Physical examination
- Laboratory investigations
History
History of present illness
-
CARDIOVASCULAR
- Hypertension
- Arrhythmias
- Ischaemic heart disease
-
RESPIRATORY
- Smoking
- COPD
- Restrictive lung disease
- (Cough, dyspnoea, chest pain - need assessment)
-
CNS
- Seizures
- Raised ICP (Intracranial Pressure)
- CVD (Cardiovascular Disease)
-
ENDOCRINE
- Diabetes Mellitus (DM)
- Thyroid conditions
- Steroid therapy
-
GI (Gastrointestinal)
- Hepatic disease
- Gastro-oesophageal reflux
-
RENAL
- Renal failure
-
HAEMATOLOGIC
- Anaemias
- Coagulopathy
HISTORY OF PAST ILLNESS
- Chronic diseases
- Jaundice
- DM (Diabetes Mellitus)
- Hypertension
- Bronchial asthma
- Emphysema
- Chronic bronchitis
Medications and allergies
Previous surgery and anaesthetics
History of alcohol, drugs, cigarette smoking
History of deep vein thrombosis
Previous postoperative nausea and vomiting
Previous difficult intubation
Family history that may affect anaesthetic management
Problems of Chronic Cigarette Smoking
- Peripheral, Coronary, and Cerebral Vascular Diseases: Chronic cigarette smoking is associated with an increased risk of vascular diseases affecting the peripheral arteries, coronary arteries, and cerebral blood vessels.
- Sympathetic Effects of Nicotine: Nicotine, a component of cigarettes, has sympathetic effects on the body, leading to conditions like hypertension (high blood pressure) and tachycardia (increased heart rate).
- Carboxy-Haemoglobin Levels: Smokers often have elevated levels of carboxy-haemoglobin in their blood. This reduces the amount of hemoglobin available for binding with oxygen, potentially compromising oxygen transport.
- Hyperactive Airways: Chronic smoking can result in hyperactive airways, leading to increased postoperative respiratory morbidity. This may manifest as bronchospasm and increased mucus secretion.
Chronic Alcoholics
Chronic alcoholics may present unique challenges in anesthesia:
- Increased Tolerance to Anaesthetic Drugs: Chronic alcoholics often develop increased tolerance to anesthesia medications due to liver enzyme induction. This can make it challenging to achieve the desired anesthetic effects.
- Hepatic and Cardiac Damage: Chronic alcoholism can lead to liver and cardiac damage, which may affect the metabolism and distribution of anesthetic agents.
- Reduced Drug Metabolism: In cases of liver damage associated with chronic alcoholism, the metabolism of drugs may be impaired, potentially affecting their clearance from the body and increasing the risk of drug interactions.
It's important for anesthesiologists to be aware of these factors when planning and administering anesthesia to patients with a history of chronic cigarette smoking or alcoholism. Tailoring the anesthesia approach to the individual patient's medical history is essential for ensuring safe and effective perioperative care.
Drug History
- ADRENALINE: Adrenaline can cause cardiac arrhythmias when used in conjunction with volatile anesthetic agents like halothane.
- AMINOGLYCOSIDES: Drugs such as streptomycin, kanamycin, gentamycin, neomycin, and tobramycin may prolong the action of non-depolarizing neuromuscular blocking drugs.
- BETA BLOCKERS: Beta blockers like propranolol, atenolol, and oxprenolol have negative inotropic effects on the heart. Caution is required when using cardiovascular depressant agents like halothane and suxamethonium in patients taking beta blockers.
- DIGOXIN: Digoxin can lead to cardiac arrhythmias when administered in conjunction with drugs like suxamethonium and halothane.
- DIURETICS: Diuretics may cause hypovolemia and hypokalemia. Hypokalemia can enhance the action of non-depolarizing neuromuscular blocking drugs.
- ANGIOTENSIN CONVERTING ENZYME (ACE) INHIBITORS: These antihypertensive drugs, such as lisinopril and captopril, can lead to severe hypotension following anesthesia induction. They may need to be withdrawn 2-3 days before surgery.
- STEROIDS: Prolonged steroid therapy (common in conditions like asthma and intracranial tumors) can suppress the hypothalamic-pituitary-adrenal axis, preventing the patient from mounting the necessary stress response to surgery. Patients on long-term steroids should receive a steroid boost in the perioperative period.
- ANTICOAGULANTS: Warfarin should be discontinued 5 days before surgery to prevent excessive bleeding.
- ANTIPLATELETS: Aspirin (e.g., Vasoprin) should be stopped 5-10 days before surgery to prevent excessive bleeding.
Steps 8 and 9 can also help to prevent epidural hematoma (spinal cord compression) following epidural or spinal anesthesia.
Family History
Family history plays a crucial role in identifying hereditary conditions associated with anaesthetic problems. These conditions must be thoroughly assessed to ensure patient safety:
- Haemoglobinopathy
- Porphyria
- Malignant Hyperthermia
- Haemophilia
- Muscular Dystrophies
Physical examination
During the preoperative assessment, a thorough examination of all body systems is essential:
- General Examination: Check for pallor, cyanosis, jaundice, edema, and ensure easy access for venipuncture.
- Respiratory System: Assess for dyspnea and listen to breath sounds.
- Cardiovascular System: Check pulse, blood pressure, and heart sounds.
Additionally, assess the ease of tracheal intubation by considering:
- Degree of mouth opening
- Condition of teeth (presence of caries, caps, loose teeth, protruding upper incisors)
- Degree of flexion of the cervical spine and extension at the atlanto-occipital joint
Problem Identification - Airway
The assessment of the airway is of utmost importance:
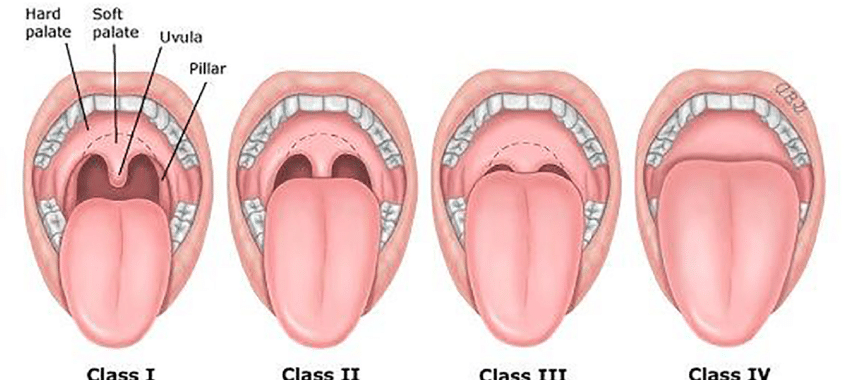
- Use the Mallampati classification to view oral and pharyngeal structures. Patients sit upright, open their jaw maximally, and protrude their tongue without phonation. Classes I, II, III, and IV indicate increasing difficulty of intubation.
- Measurements to consider:
- Interincisor distance: < 3 cm (indicative of difficult intubation)
- Thyromental distance: < 6.5 cm (indicative of difficult intubation)
- Sternomental distance: < 12.5 cm (indicative of difficult intubation)
Mallampati Classification
The Mallampati Classification is used to assess the visibility of oral and pharyngeal structures, which can help predict the difficulty of tracheal intubation:
- Class I: Soft palate, uvula, anterior, and posterior faucial pillars are visible.
- Class II: Soft palate and uvula are visible.
- Class III: Soft palate and the base of the uvula are visible.
- Class IV: Soft palate is not visible.
Laboratory investigations
Preoperative Investigations - Guidelines
1. Urinalysis: Perform on all patients. It's cost-effective and may reveal conditions like diabetes mellitus (DM) or urinary tract infection (UTI).
2. Hemoglobin (Hb) or Hematocrit (PCV): Recommended for all patients.
3. Serum Electrolytes (E & U): Required in patients with diarrhea, vomiting, metabolic disease, renal or hepatic issues, and major surgeries. Also, for patients on diuretics, digoxin, antihypertensives, steroids, or hypoglycemic agents.
4. Chest X-ray (CXR): Recommended for elderly patients and those with respiratory or cardiac diseases.
5. Electrocardiogram (ECG): Essential for patients over 50 years old and those with cardiovascular (CVS) disease or diabetes mellitus (DM).
6. Sickle Cell Status: Particularly relevant in environments where sickle cell disease is prevalent.
7. Additional tests: Depending on the patient's history and examination, other tests may be necessary. For example, blood sugar tests for DM or steroid therapy, pulmonary function tests (PFTs) for chronic obstructive pulmonary disease (COPD) or asthma, and coagulation screening for liver disease or severe pre-eclampsia.
Risk Assessment
The risk assessment is used to determine whether a patient is in optimal condition for the proposed surgery. The American Society of Anesthesiologists’ (ASA) physical status classification is commonly used. It originally had five categories, and a sixth was later added to address the brain-dead organ donor.
| ASA CLASS | DEFINITION |
|---|---|
| 1 | A normal healthy patient |
| 2 | A patient with mild systemic disease (no functional limitations) |
| 3 | A patient with severe systemic disease (some functional limitations) |
| 4 | A patient with severe systemic disease that is a constant threat to life (function incapacitated) |
| 5 | A moribund patient who is not expected to survive without the operation |
| 6 | A brain dead patient whose organs are being removed for donor purposes |
If the procedure is an emergency, the physical status is followed by the letter 'E' (e.g. 3E).
Fasting Guidelines
For all age groups:
- Clear fluids: 2 hours
- Breast milk: 4 hours
- Infant formula: 6 hours
- Non-human milk: 6 hours
- Light meal: 6 hours
Avoid starvation and dehydration in children.
Preoperative Preparation
Patients with diseases such as cardiac, respiratory, diabetes mellitus, hypertension, thyrotoxicosis, haemoglobinopathy, and emergency surgical cases may need further appropriate investigations to assess their suitability for the proposed surgery and stabilization (optimization) before surgery. Blood grouping and cross-matching may be indicated.
Physiological variables may need to be improved with:
- Intravenous fluids (crystalloids, colloids) and blood may be needed to optimize the cardiovascular system following hemorrhage.
- Inotropic drugs (dobutamine, dopamine) to support the compromised cardiovascular system.
- Vasodilators (glyceryl trinitrate, hydralazine, sodium nitroprusside) in cases of severe hypertension.
Preoperative Preparation Checklist
- Remove nail varnish, lipstick, and cosmetics as they may mask pallor and cyanosis.
- Remove rings, necklaces, and earrings from the patient.
- Ensure the patient's identification label and case folder accompany them to the theatre.
- Mark the eye or limb to be operated on, and indicate all bilateral organs to be operated on directly on the patient's body.
- Obtain written informed consent from the patient for the proposed surgery.
Practice Questions
Check how well you grasp the concepts by answering the following questions...
Practice Essay Questions:
- Discuss the importance of preoperative assessment in ensuring patient safety and optimal perioperative care. Highlight key objectives and considerations in this process.
- Examine the impact of chronic cigarette smoking and alcoholism on anesthesia. What challenges do these factors pose, and how can anesthesiologists tailor their approach to ensure safe perioperative care for such patients?
- Analyze the role of family history in identifying hereditary conditions associated with anesthesia-related problems. How can a thorough assessment of family history contribute to enhanced patient safety?
- Explain the significance of drug history in anesthesia. Provide examples of specific drugs and their potential interactions that an anesthesiologist should be aware of during preoperative assessment.
- Explore the steps involved in a comprehensive physical examination during preoperative assessment. How does this examination contribute to the overall assessment of a patient's fitness for surgery and anesthesia?
- Evaluate the Mallampati Classification system for airway assessment. How does it help predict the difficulty of tracheal intubation, and what measurements are considered in this classification?
- Interpret the guidelines for preoperative laboratory investigations, including urinalysis, hemoglobin, electrolytes, chest X-ray, and ECG. How do these investigations contribute to the overall assessment of a patient's suitability for surgery?
- Utilize the ASA Physical Status Classification to assess a patient's risk for surgery. Discuss the different ASA classes and their implications for perioperative care.
- Discuss the fasting guidelines for different age groups before surgery. Why is it important to adhere to these guidelines, and how can they contribute to the safety and success of a surgical procedure?
- Examine the importance of preoperative preparation in patients with specific medical conditions. How can intravenous fluids, inotropic drugs, and vasodilators be used to optimize physiological variables before surgery?
Practice Short Answer Questions:
- Name three factors considered during the assessment of a patient's airway in the Mallampati Classification system.
- Briefly explain the significance of the ASA Physical Status Classification in the context of preoperative assessment.
- List three examples of drugs mentioned in the text that may have interactions with anesthesia agents and pose challenges in perioperative care.
- What physiological variables may need to be improved with intravenous fluids and blood in the preoperative preparation of a patient?
- Explain the fasting guidelines for clear fluids and breast milk before surgery in pediatric patients.
- Why is a family history assessment crucial in identifying hereditary conditions associated with anesthesia problems?
- What are the main objectives of preoperative assessment, and how do they contribute to improved outcomes and patient satisfaction?
- Describe the Mallampati Classification Class III. What does it indicate regarding the visibility of oral and pharyngeal structures?
- What does the term "ASA Class 4" mean, and how does it impact the planning of perioperative care?
- In the context of preoperative preparation, why is it important to remove nail varnish, lipstick, and cosmetics from the patient?
Contributors
Jane Smith
She is not a real contributor.
John Doe
He is not a real contributor.
Send your comments, corrections, explanations/clarifications and requests/suggestions