What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
- Peptic ulcer disease is a spectrum that covers GERD, DU, GU, Gastritis, ZES resulting from the action of acid/pepsin on vulnerable epithelium.
- Commonly occurs in the
- lower esophagus
- stomach
- duodenum
- jejunum
- Meckel’s diverticulum with ectopic gastric epithelium
- Commonest sites are the 1st part of duodenum and the lesser curvature of the stomach.
Anatomy
The stomach is a J-shaped organ that digests food. It consists of four parts:
- Cardia
- Fundus
- Body
- Pylorus
Gross Anatomy
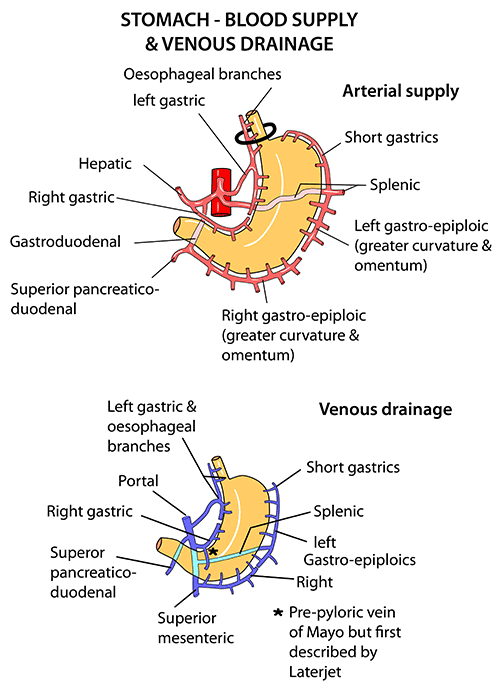
The stomach's blood supply:
- Mainly from the celiac trunk.
- Left gastric
- Right gastric
- Right gastroepiploic branches of the hepatic
- Left gastroepiploic
- Short gastric branches
Histology
Histologically, the stomach is divided into three regions:
- Cardia
- Fundus
- Pylorus
- Mucosa
- Submucosa
- Muscularis externa
- Serosa
Physiology
The stomach serves as a temporary holding chamber, allowing you to ingest a meal far more quickly than it can be digested and absorbed by the small intestine 56. It mixes food with stomach acid and breaks food down into smaller particles using chemical and mechanical digestion 56. Additionally, the stomach also absorbs water.
Gastric Juice
- Composed of hydrochloric acid (HCl), pepsinogen, intrinsic factor (IF), and mucus.
- HCl and pepsinogen initiate protein digestion.
- IF is required for vitamin B12 absorption in the ileum.
- Mucus protects the gastric mucosa from the corrosive action of HCl.
- Other components of gastric juice include:
- Gastrin (G cells)
- Histamine (ECL cells)
- Somatostatin (D cells)
- Prostaglandins
- Blood group antigen
- Electrolytes
Stimulation of Gastric Acid Secretion
Cephalic Phase: This phase is vagally mediated and is triggered by the sight, smell, and taste of food. The brain sends signals via the vagus nerve to stimulate the gastric glands in the stomach wall to secrete gastric juice.
Gastric Phase: This phase begins when food arrives in the stomach. The presence and distension of the stomach by food stimulate gastric activity. About two-thirds of gastric juice is secreted during this phase.
Intestinal Phase: This phase begins when food leaves the stomach and enters the small intestine. It helps to control the rate of gastric emptying to ensure that the secretory, digestive, and absorptive capacities of the duodenum are not overwhelmed.
Inhibition of Gastric Acid Secretion
Inhibition of Gastrin Release: When the pH of the stomach is less than 2, gastrin release is inhibited. This is a negative feedback mechanism to prevent the overproduction of gastric acid.
Intestinal Inhibition by Hormones: Certain hormones released in the intestines, such as Cholecystokinin (CCK) and Vasoactive Intestinal Peptide (VIP), can inhibit gastric acid secretion. These hormones help to coordinate the digestive processes among different parts of the digestive tract.
The regulation of gastric acid secretion is complex and involves extensive coordination between the gut and brain. It reflects an intricate balance of chemotransmitters delivered to the gastric mucosa by several pathways that mediate both stimulatory and inhibitory mechanisms.
- Definition: A break in the mucosa of the stomach, 1st part of the duodenum, lower esophagus extending into the submucosa or deeper.
- Can be acute or chronic.
- Results from the action of acid/pepsin on vulnerable epithelium.
- Results from an imbalance between mucosa defenses and aggressive factors.
- Occurs in about 4% of the population.
- Causes include H-pylori infection, NSAID use, stress, gastrinoma, increased acid/pepsin levels, etc.
Aggressive Factors
- H. pylori: This bacterium can cause chronic inflammation and ulcers in the stomach.
- NSAIDs: Long-term use of nonsteroidal anti-inflammatory drugs can lead to peptic ulcer disease.
- Stress, Acid/Pepsin, Steroids, Alcohol, Cigarette: These factors can increase the production of stomach acid, disrupt the protective lining of the stomach, and lead to ulcers.
Defense Mechanisms
- Mucous and Bicarbonate: These substances form a protective barrier in the stomach lining.
- Blood Flow: Adequate blood flow is essential for maintaining the health of the stomach lining.
- Cell Junction and Apical Resistance: These cellular structures help maintain the integrity of the stomach lining.
- Regeneration: The stomach lining has a high capacity for regeneration, which is crucial for healing ulcers.
Repair Processes
- Restitution: This is the initial phase of healing where the cells surrounding the ulcer change shape and spread to cover the wound.
- Mucoid Cap Formation: This involves the formation of a protective layer over the ulcer.
- Proliferation: This is the phase where new cells are produced to replace the damaged ones.
- Growth Factor: These proteins stimulate cell growth and play a crucial role in wound healing.
- The majority of DU/GU is caused by H. pylori infection (90-95%) and NSAIDs.
- The final pathway to ulcer formation is acid-pepsin injury of the gastroduodenal mucosal barrier.
- Acid suppression is the mainstay of healing and preventing recurrence.
- NSAIDs cause ulceration by compromising mucosal defense.
- H. pylori causes ulceration through inflammation, compromise of mucosal defense mechanisms, and acid hypersecretion.
H. pylori
- A specialized flagellate, capable of navigating and attaching to apical cells, rich in urease.
- Approximately 50% of the world population is affected by H. pylori.
- Splits urea to ammonia, damaging the surface epithelial cells and bicarbonate that encourage acid secretion.
- Produces toxins, cytokines, inflammatory and mediatory cells, thereby weakening the mucosal defenses.
Gender and Age
- Duodenal Ulcers (DU): More common in men than women with a ratio of 2:1.
- Gastric Ulcers (GU): Occur equally in men and women (ratio 1:1). GU patients are generally older, possibly due to increased NSAID use in old age.
Symptoms
- Abdominal Pain: The most common symptom is a burning pain in the epigastric region.
- DU: Pain often occurs at night or 2-3 hours after a meal and may wake the patient.
- GU: Pain is often associated with eating.
- Other symptoms can include nausea, bloating, belching, reflux, weight loss, anemia, and positive occult blood.
Complications
Complications can include upper gastrointestinal (UGI) bleeding, perforation, peritonitis, shock, and gastric outlet obstruction (GOO). These complications are serious and require immediate medical attention.
Diagnosis
The diagnosis of peptic ulcers involves a combination of clinical history, physical examination, and various diagnostic tests.
Differential Diagnosis
Peptic ulcer disease must be differentiated from other conditions that present with similar symptoms. These include:
- Esophagitis/Gastritis due to alcohol, NSAIDs, or stress
- Hiatus hernia
- Barrett’s esophagus
- Gastroesophageal reflux disease
- Acute pancreatitis
- Primary biliary cirrhosis
- Cholelithiasis
- Gastric outlet syndrome
- Myocardial infarction
- Pleural empyema
- Acute appendicitis
Investigations
Several investigations can be used to diagnose peptic ulcers and determine their cause:
- Endoscopy: This allows direct visualization of the ulcer and can also be used to obtain biopsy samples.
- Contrast X-ray Studies: These can help visualize the gastrointestinal tract and detect abnormalities.
- Ultrasonography: This can be used to visualize the abdominal organs and detect any abnormalities.
- H. pylori Test: This can be done using blood tests, breath tests, or stool tests to detect the presence of H. pylori bacteria.
- Abdominal CT/MRI: These imaging techniques can provide detailed images of the abdominal organs.
- Laparoscopy: This is a surgical procedure that allows the doctor to view the organs in the abdomen.
- Angiography: This is used to visualize the blood vessels in the stomach.
- Emptying Studies: These can help determine how quickly food leaves the stomach.
- Gastric Acid Secretion Tests: These can help determine the amount of acid
Protective Measures
- Antacids: Over-the-counter medications that neutralize gastric acid, providing symptomatic relief.
- Cytoprotection: Agents such as sucralfate and misoprostol provide a protective barrier to the gastric mucosa.
- Prostaglandin Analogues: Medications like misoprostol enhance mucosal defenses, particularly in patients on NSAIDs.
Acid Reduction
- Proton Pump Inhibitors (PPIs): Medications like omeprazole, lansoprazole, and pantoprazole inhibit the H+/K+ ATPase enzyme system at the secretory surface of gastric parietal cells, reducing gastric acid secretion.
- H2 Receptor Antagonists: Medications like ranitidine and famotidine block histamine at the H2 receptors of gastric parietal cells, inhibiting gastric acid production.
H. Pylori Treatment
Eradication therapy typically involves a combination of antibiotics (e.g., amoxicillin, clarithromycin) and a PPI to eliminate H. pylori, the most common etiological agent of peptic ulcers.
NSAID Cessation
If NSAIDs are implicated in ulcerogenesis, cessation or substitution with a COX-2 selective NSAID may be recommended.
Supportive Measures
Lifestyle modifications, including smoking cessation and alcohol reduction, can mitigate symptoms and prevent ulcer recurrence.
Surgical Intervention
Indicated in cases of complications such as bleeding, perforation, obstruction, intractability, or non-healing ulcers.
SURGICAL INTERVENTIONS INCLUDE-
Simple Over Sewing of Bleeding Ulcer
This is a surgical procedure used to treat bleeding peptic ulcers. The surgeon uses sutures to close the ulcer, which helps stop the bleeding.
Simple Patch Closure of Perforation
In this procedure, a perforated peptic ulcer is sealed by suturing a patch of tissue (usually from the omentum, a fatty apron-like structure that hangs off the stomach) over the perforation.
Distal Gastrectomy + GD or GJ
Distal gastrectomy involves the removal of the lower part of the stomach, often due to a peptic ulcer or stomach cancer. GD (gastro-duodenostomy) or GJ (gastro-jejunostomy) refers to the method of reattaching the remaining stomach to the digestive tract.
Vagotomy
This is a surgical procedure where parts of the vagus nerve are cut to reduce acid secretion in the stomach, thereby helping to prevent peptic ulcers. There are different types of vagotomy, including truncal, selective, and highly selective vagotomy (HSV), each with different effects.
Vagotomy + Distal Gastrectomy
This combines the two procedures above. The lower part of the stomach is removed, and the vagus nerve is cut to reduce acid secretion.
GJ Only
This refers to a gastrojejunostomy without any other procedures. It’s a surgical procedure that connects the stomach directly to the jejunum (part of the small intestine) to allow food to bypass the duodenum.
Endoscopy: Ballooning, Injection Sclerotherapy
Endoscopic procedures are minimally invasive and can be used to treat peptic ulcers. Ballooning (also known as dilation) is used to widen a narrowed area. Injection sclerotherapy involves injecting a solution into the blood vessels to stop bleeding.
| Operative mortality, morbidity and recurrence rates for peptic ulcer operations | |||
|---|---|---|---|
| Operation | Mortality | Morbidity | Recurrence |
| Gastrectomy | 1-2% | 20-40% | 1-4% |
| GJ | < 1 | 10-20 | 50 |
| TV + drainage | < 1 | 10-20 | 2-7 |
| SV + drainage | < 1 | 10-20 | 5-10 |
| HSV | < 0.2 | < 5 | 2-10 |
| TV+ antrectomy | 1 | 10-20 | 1 |
GERD arises due to a mechanically defective Lower Esophageal Sphincter (LES). This defect leads to an increased exposure of the esophagus to fluid with a pH less than 4 and greater than 7.
GERD is the precipitating cause of chronic esophagitis, an inflammation of the esophagus.
Attenuation of the collar string musculature leads to the opening of the gastric cardia and loss of the high-pressure zone. This results in the reflux of gastric contents into the esophagus.
The damage in GERD is caused by acid, pepsin, and biliary and pancreatic secretions from the stomach. These substances can irritate and damage the lining of the esophagus.
Gastroduodenal reflux, which involves both gastric acid and duodenal bile, is often worse than gastric reflux alone. This is because bile salts in the refluxate can damage the esophageal mucosa.
Clinical Features
- Heartburn: Substernal burning discomfort in the epigastrium, typically postprandial and responsive to antacids.
- Regurgitation: Retrosternal return of gastric contents into the mouth, not preceded by nausea.
- Dysphagia: Difficulty in swallowing, suggestive of esophageal motility disorder or stricture.
Diagnosis
Primarily clinical, based on characteristic symptomatology. Empirical trial of proton pump inhibitors (PPIs) often diagnostic.
Investigation
Upper Gastrointestinal Endoscopy: Gold standard for visualizing mucosal lining, identifying complications (e.g., esophagitis, Barrett’s esophagus).
Medical Treatment
- Antacids: Neutralize gastric acid, providing symptomatic relief.
- Protective Barrier: Agents such as sucralfate provide a protective barrier to the gastric mucosa.
- Anti-secretory/Suppression: Proton Pump Inhibitors (PPIs) inhibit the H+/K+ ATPase enzyme system at the secretory surface of gastric parietal cells, reducing gastric acid secretion.
Supportive Measures
Lifestyle modifications can mitigate symptoms and prevent GERD recurrence. These include avoiding late dinners, tight clothing, elevating the head during sleep, and reducing alcohol and cigarette consumption.
Surgical Treatment
- Laparoscopic Anti-Reflux Surgery: Minimally invasive surgery strengthens the lower esophageal sphincter to prevent acid reflux.
- Nissen Fundoplication: Procedure involves wrapping the upper part of the stomach around the lower end of the esophagus to reinforce the lower esophageal sphincter.
- Toupet & Belsey Mark IV: Variations of fundoplication procedures used to treat GERD.
Prognosis
GERD typically requires lifelong treatment to manage symptoms and prevent complications.
Complications
Long-term complications associated with GERD include esophagitis, stricture, Barrett’s Esophagus (BE), and aspiration.
Definition: Gastritis refers to inflammation of the gastric mucosa.
Causes: The etiology of gastritis is multifactorial and includes:
- H. pylori infection: The most common cause of chronic gastritis worldwide.
- Alcohol: Can cause acute and chronic gastritis.
- NSAIDs: Non-steroidal anti-inflammatory drugs can lead to gastritis by disrupting the stomach’s protective mucosal barrier.
- Crohn’s disease: Although primarily a disease of the small intestine, Crohn’s disease can involve the stomach and cause gastritis.
- Tuberculosis (TB): Gastric TB is rare but can cause gastritis.
- Bile reflux: Backflow of bile into the stomach can cause gastritis.
Clinical Types:
- Acute Gastritis: Rapid onset of symptoms, often due to NSAIDs or alcohol. Can be classified as Type A (autoimmune) or Type B (H. pylori).
- Stress Ulceration: Acute mucosal ulceration that occurs in response to severe physiological stress such as trauma (burns, head injury), sepsis, hypotension, jaundice, or renal failure.
ZES is a condition characterized by gastric acid hypersecretion due to a gastrin-producing tumor, known as a gastrinoma. This results in intractable duodenal ulceration.
Etiology
The condition is caused by the uncontrolled secretion of an abnormally increased amount of gastrin by a tumor of non-B islet cells of the pancreas (80%) or duodenum (20%), which are neuroendocrine tumors.
- 80% of cases are sporadic.
- 20% are inherited and are associated with Multiple Endocrine Neoplasia type 1 (MEN 1), which involves tumors of the parathyroid, pituitary, and pancreatic/duodenal glands.
- 50-60% of cases result from malignant gastrinomas.
Clinical Features
- There is a male preponderance.
- Patients often experience intractable pain.
- A history of previous surgery for an ulcer is common.
- Fulminant cases may present with hematemesis, perforation, and gastric outlet obstruction (GOO).
- Diarrhea is seen in 30% of cases, often accompanied by dehydration and hypokalemia.
- The diarrhea is due to excess acid into the duodenum, damaging the intestinal mucosa, and steatorrhea from inactivation of lipase by the acid.
- Gastroesophageal Reflux Disease (GERD) is also common.
- Peptic Ulcer Disease (PUD) is seen in 90% of cases.
Investigations
- General Work Up: Includes a thorough medical history and physical examination.
- Upper Gastrointestinal (UGI) Endoscopy: Allows for direct visualization of the esophagus, stomach, and duodenum.
- Abdominal Imaging: Ultrasonography (USS), Computed Tomography (CT), and Magnetic Resonance Imaging (MRI) can help identify the presence and location of gastrinomas.
- Gastrin Secretion Tests: Overnight volume > 1000mls, Basal Acid Output (BAO) > 15mmol.
- Serum Gastrin: Elevated in patients with ZES.
- Serum Calcium: Hypercalcemia may suggest the presence of Multiple Endocrine Neoplasia type 1 (MEN 1).
- Secretin Provocative Test: An increase in gastrin levels after administration of secretin is a positive result indicative of ZES.
- Parathyroid Hormone: Elevated levels can help confirm the diagnosis of MEN 1.
Treatment
- Medical: H2 blockers and Proton Pump Inhibitors (PPIs) to reduce gastric acid secretion.
- Supportive Measures: Includes dietary modifications and lifestyle changes.
- Surgery: Resection when the gastrinoma is solitary. Procedures can include laparotomy, enucleation, distal pancreatectomy, Whipple’s procedure, total gastrectomy, and highly selective vagotomy (HSV).
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions