What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
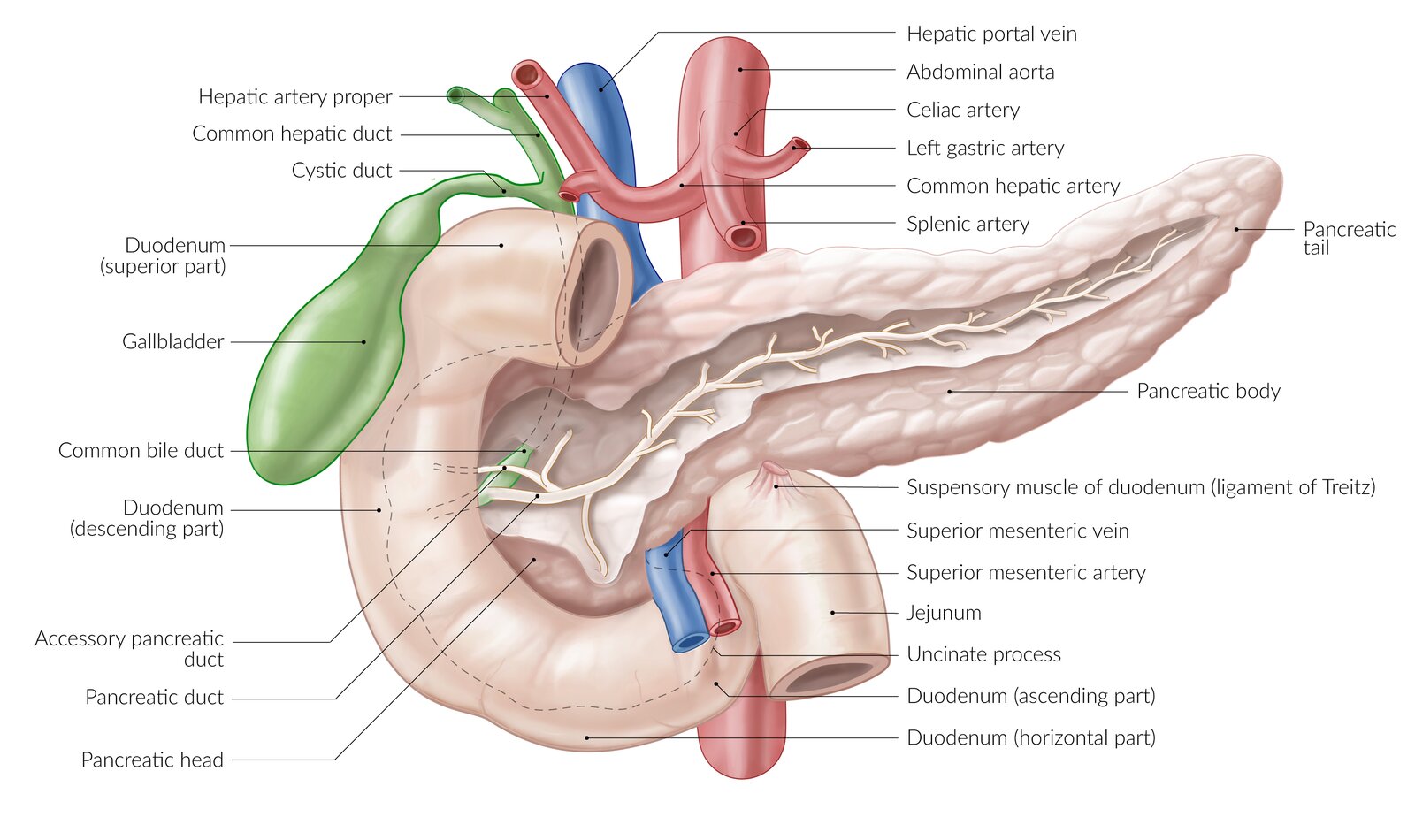
Soft, lobulated gland about 12-15cm in length
- Transversely Retroperitoneal
- Between C loop of Duodenum and Spleen
- Behind the stomach
- Divided into: Head / Neck / Body / Tail
- Consists of Exocrine and Endocrine glands
- Exocrine secretions: Drained by pancreatic duct which joins the common bile duct to empty into 2nd part of duodenum at the duodenal papilla
- Blood supply: Celiac trunk and superior mesenteric arteries
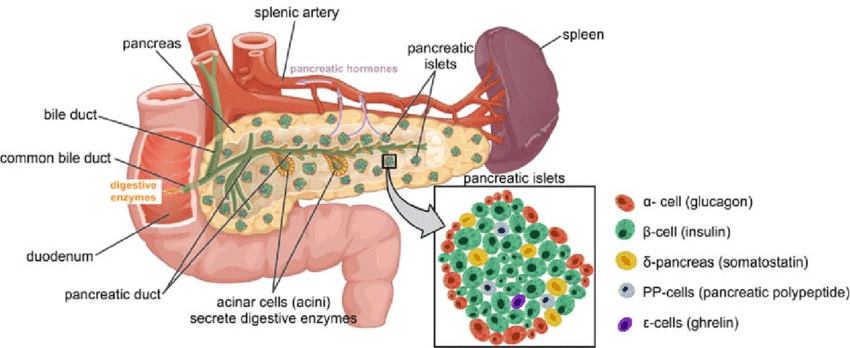
Exocrine:
- Secretes 2.5 liters protein-rich alkaline Enzymes
- Enzymes include: Trypsinogen / Amylase / Lipase / Ribonuclease
- Also secretes: Electrolytes
- Secretion is stimulated by: Secretin and cholecystokinin
Endocrine:
- Insulin
- Glucagon
- Somatostatin
- Serum/Urinary Pancreatic Enzyme Estimation
- Abdominal Ultrasonography
- Plain Radiography
- Computerised Tomography/Contrast-enhanced Magnetic Resonance Imaging
- Endoscopic Retrograde Cholangiopancreatography
- Pancreatic exocrine function test
Inflammatory and Necrotic disorder of the pancreas
- Acinar cell destruction: Caused by autodigestion from intra-parenchymal activation of pancreatic enzymes
- Premature activation of trypsin: Causes parenchymal inflammation/necrosis
Relatively uncommon diagnosis in this environment
Etiology
- Biliary tract stone disease
- Alcohol (Ethanol) abuse: 70-80% of cases are due to these two causes
- Medications: Steroids / Isoniazide / Enaleprine
- Hyperlipidemia
- Pancreatic duct obstruction
- Hereditary/Genetic pancreatic enzyme anomaly
- ERCP/Endoscopic maneuvers around the sphincter of Oddi
- Autoimmune disease
- Trauma
- Toxins
- Hypercalcemia
Presentation
Epigastric abdominal pain of acute onset
- May involve adjacent quadrants
- May radiate to the back.
- Pain is constant
- May be relieved by leaning forwards
Nausea and Vomiting
- May be associated with Mallory Weiss tear
On Examination
- Restless
- Mild fever
- Dehydrated / Hypovolemic
- Tachypnea
- Mild to moderate Jaundice
- Altered sensorium
- Abdominal distension / Tender with rebound / Tympanitic / Hypoactive bowel sounds
- Epigastric tender mass
- Flank Ecchymosis (Grey Turner's syndrome) / Periumbilical Ecchymosis (Cullen's syndrome)
Investigations
- Elevated Serum Amylase/Lipase
- Elevated Urinary Amylase
- Other Blood tests:
- Hematocrit
- Electrolytes and urea
- Glucose
- Bilirubin
- Triglyceride
- Calcium
- Abdominal Ultrasound: May reveal pancreatic edema / Gall or biliary stones
- Plain Chest / Abdominal radiography:
- Rule out Pneumonia / perforated hollow viscus/int obstruction
- Contrast-enhanced Computerized Tomography
- MRI
- Pancreatic Edema
- Pancreatic necrosis
- Intra/peri pancreatic fluid accumulation
- ERCP
Differential Diagnosis
- Cholecystitis
- Cholangitis
- Perforated hollow viscus
- Intestinal obstruction
- Mesenteric ischemia/Infarction
Treatment
- Fluid/Electrolyte resuscitation
- Pain control
- Naso-gastric decompression
- Nutrition
- Prophylactic antibiotics
- Cholecystectomy/bile duct exploration
Complications
- Pancreatic Necrosis
- Infected Pancreatic Necrosis
- Pancreatic Pseudocyst
- Pancreatic Abscess
- Splenic Vein thrombosis
- Chronic Pancreatitis
Chronic progressive inflammation and destruction of the Pancreas. Characterized by pancreatic fibrosis and loss of pancreatic function.
Exocrine/Endocrine:
- Associated with enlargement and hardening of pancreas from fibrosis
- Duct distortion/Strictures
- Intraductal calcification
Rare in this environment.
Presents with chronic epigastric pain / pancreatic insufficiency / obstructive jaundice. Associated with recurrent episodes of acute pancreatitis causing worsening pain.
Most frequently caused by alcoholism. Pancreatic duct obstruction from trauma / acute pancreatitis / Cancer. Hereditary pancreatitis / Idiopathic.
Clinical Features
- Moderate to severe abdominal pains
- Weight loss
- Insomnia
- Abuse of analgesics
- Steatorrhea
- Diabetes mellitus
Investigations
- Raised serum amylase in early presentation
- Abnormal pancreatic function tests
- MRI
- CT
- ERCP / Percutaneous pancreatogram
- MR cholangiogram / pancreatogram
Treatment
- Analgesia
- Abstinence from alcohol
- Low-fat diet
- Pancreatic enzyme supplementation
Indication for surgery:
- Duct obstruction
- Removal of mass lesions in the head of pancreas
Complications
- Includes all possible complications of acute pancreatitis
- Pancreatic carcinoma
Disease of the elderly. Equal male-to-female ratio.
Predisposing Factors
- Smoking
- Chronic pancreatitis
- More than 85% - ductal adenocarcinoma
Symptoms
Non-specific:
- Epigastric discomfort / pain
- Anorexia
- Weight loss
- Jaundice with hepatomegaly and enlarged palpable gall bladder
Treatment
Surgery
- Curative but possible in less than 10%:
- Pancreatoduodenectomy
- Palliative:
- Cholecystojejunostomy
- Choledochojejunostomy
Stenting
- Endoscopic
- Percutaneous
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions