What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
Any condition that interferes with the normal propulsion and passage of intestinal contents.
Can involve the small bowel, colon, or both small bowel and colon, as in generalized ileus.
- Cause of obstruction: Mechanical or functional (Ileus).
- Duration of obstruction: Acute or chronic.
- Extent of obstruction: Partial or complete.
- Type of obstruction: Simple or complex (closed loop and strangulation).
Neonate
- Anorectal malformation: 43%
- Hirschsprung’s disease: 18.7%
- Jejunoileal atresia: 15.6%
- Duodenal atresia: 7.8%
- Hernia: 6.3%
Children
- Incarcerated Hernia: 50%
- Intussusception: 37%
- Postop Adhesion: 13%
- Distal obstruction
- Proximal dilatation/abdominal distention:
- Vascular compromise: Ischemia, perforation, gangrene
- Vomiting
- Dehydration
Intestinal obstruction usually presents with:
- Vomiting
- Abdominal distention
- Constipation
- Pain/Excessive crying
History
A thorough history is essential in evaluating a child with suspected intestinal obstruction. Key aspects include:
Onset and Duration of Symptoms
Determine the time of onset and progression of symptoms, such as abdominal pain, vomiting, distension, and failure to pass stool or flatus. Acute onset may suggest volvulus or intussusception, whereas a more insidious onset could indicate congenital anomalies or chronic conditions.
Character of Vomiting
Ascertain whether vomiting is bilious or non-bilious. Bilious vomiting is suggestive of obstruction distal to the ampulla of Vater, which is a surgical emergency.
Pain Characteristics
Identify the nature, location, and radiation of abdominal pain. Colicky pain often indicates mechanical obstruction, whereas continuous pain might suggest ischemia or perforation.
Stool and Flatus Passage
Inquire about the last passage of stool and flatus. Absolute constipation indicates a distal obstruction, whereas partial obstruction may still allow for some passage.
Previous Episodes
Ask about any previous similar episodes, surgeries, or medical conditions. Previous surgeries increase the risk for adhesions, which are a common cause of obstruction.
Feeding History and Growth
For infants, a detailed feeding history and growth chart review can provide clues to chronic obstruction or congenital anomalies.
Family History
Consider any family history of conditions like Hirschsprung's disease, cystic fibrosis, or other congenital anomalies that may predispose the child to bowel obstruction.
Physical Examination
A comprehensive physical examination should be performed with attention to:
General Appearance
Assess for signs of distress, dehydration, and shock. Look for pallor, lethargy, or irritability.
Abdominal Examination
- Inspection: Look for distension, visible peristalsis, scars, and any external signs of congenital anomalies.
- Auscultation: Evaluate bowel sounds, which may be hyperactive in early obstruction and hypoactive or absent in late stages or with peritonitis.
- Palpation: Perform gentle palpation to identify tenderness, guarding, or masses. A sausage-shaped mass may suggest intussusception. Rebound tenderness indicates peritoneal irritation.
- Percussion: Check for tympany indicating gas-filled loops or dullness suggesting fluid accumulation.
Rectal Examination
Perform to check for impacted stool, blood, or masses. A forceful expulsion of air and stool upon withdrawal of the finger (explosive stool) can indicate Hirschsprung’s disease.
Systemic Examination
Include examination of other systems to rule out associated congenital anomalies or systemic illnesses that may present with intestinal obstruction.
Investigation
Investigations aim to confirm the diagnosis, determine the cause, and assess the severity of obstruction:
Laboratory Tests
- Full Blood Count (FBC): To check for leukocytosis indicative of infection or inflammation.
- Electrolytes and Renal Function Tests: To assess dehydration and electrolyte imbalances.
- C-Reactive Protein (CRP) and Procalcitonin: Markers of inflammation and sepsis.
- Blood Gas Analysis: To evaluate metabolic acidosis, which can occur with bowel ischemia.
Imaging
- Plain Abdominal X-Ray: The initial imaging modality to identify air-fluid levels, dilated bowel loops, and absence of gas in the distal bowel. A classic "double bubble" sign indicates duodenal atresia, while a "target sign" may suggest intussusception.
- Ultrasound: Useful for diagnosing intussusception, identifying free fluid, and evaluating for appendicitis or other intra-abdominal masses.
- Contrast Enema: Both diagnostic and therapeutic in intussusception. It can outline the colon and identify areas of obstruction.
- Upper GI Series with Small Bowel Follow-Through: To evaluate for malrotation with midgut volvulus, particularly in infants with bilious vomiting.
- CT Scan: Considered in unclear cases or to evaluate for complications like perforation or abscess. It provides detailed information about the location, cause, and complications of obstruction.
Additional Tests
- Stool Tests: For occult blood or pathogens if an infectious cause is suspected.
- Genetic Testing: In cases with a suspected hereditary component like cystic fibrosis or Hirschsprung’s disease.
Treatment
Goals:
- Relief of obstruction
- Restoration of normal bowel function with minimal morbidity and negligible mortality
Resuscitation
- Decompression
- Fluid rehydration
- Correct electrolyte imbalance
Definitive Treatment
Depends on the cause
- Malrotation
- Intestinal atresia
- Hernia
- Intussusception
- Hirschsprung’s disease
- Anorectal malformation (ARM)
- During 6-12 week of gestation, the intestine undergoes evisceration, elongation, and eventual return to the abdominal cavity in a 270 degree counterclockwise rotation with fixation.
- Malrotation is associated with abnormal rotation and fixation.
- Most develop symptoms in first month of life.
- If patient stable do UGI series (gold standard).
- See bird’s beak in third part of duodenum.
- Ligament of Treitz is right of midline.
- Midgut volvulus is a surgical emergency.
- Volume resuscitation is essential.
- If patient in shock, no studies are warranted.
Treatment
- Surgical
- Ladd’s procedure
- Duodenal
- Jejunoileal
- Colonic
Duodenal Atresia
- Failure of recanalization during 8-10th week of gestation.
- Presents in first 24hrs of life.
- Trisomy 21 is present in about 25%.
- Characterized by bilious emesis.
- Abdominal distension is absent.
- 85% distal to ampulla of vater.
- Surgical treatment is a duodenoduodenostomy.
Jejunoileal Atresia
- Jejunoileal atresia is caused by an in utero vascular accident.
- Presents within first 2-3 days.
- Associated with Cystic Fibrosis in 10%.
- Treatment
- Resuscitation
- Resection and anastomosis
Definition: Protrusion of viscera through a defect in the wall of its containing cavity
How common are hernias?
- About 1-5% of babies develop hernias.
- Boys are 10 times more likely than girls to have a hernia.
- Hernias are found in as many as 30% of prematurely born babies.
Symptoms:
- Swelling or visible lump in groin
- Swelling in the scrotum
- The swelling:
- Is usually painless (but may have some mild discomfort)
- Soft and smooth in texture
- May disappear or reduce in size when baby is relaxed and lying flat
- May appear or increase in size when baby is crying, coughing, or straining
Inguinal Hernia
Consequence
- Irreducible/ Incarceration
- Obstruction
- Strangulation
Monitor for incarceration/obstruction:
- Child appearing ill
- Pain in the groin
- Nausea and vomiting
- Bloating or full abdomen
- Fever
- Swelling that appears red or dusky in color and is markedly tender
- Swelling that does not change in size when crying
Treatment
- Surgery is necessary in all cases, even if it is not yet incarcerated.
- Surgery – Herniotomy
- Herniotomy will prevent complication.
- Recurrence rates are less than 1% in an uncomplicated hernia.
- Most occur before age of two.
- Etiology is thought to be lymphoid hyperplasia in terminal ileum after a viral illness.
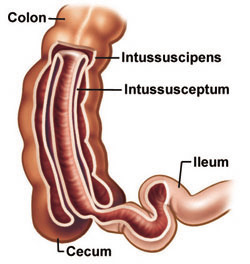
- Proximal bowel (intussusceptum) invaginates into the distal bowel (intussuscipien) causing swelling, obstruction, and possible vascular compromise.
Types:
- Ileocolic
- Colo-colic
- Ileo-ileal
Pathophysiology
- Compression of mesentery
- Venous engorgement
- Edema
- Ischemia of intestinal mucosa
- Gangrene and perforation
Presentation
History
Intussusception is a serious condition characterized by the telescoping of a proximal segment of the intestine (the intussusceptum) into a distal segment (the intussuscipiens), resulting in bowel obstruction and potential compromise of blood supply. Its presentation typically includes:
- Sudden Onset Colicky Abdominal Pain: Often described by caregivers as severe, episodic pain, with pain-free intervals.
- Vomiting: Frequently bilious and recurrent due to the obstructive nature of the condition.
- Bloody Mucous Stools (Currant Jelly Stools): The presence of blood and mucous in stools is pathognomonic, indicative of intestinal mucosal edema, venous congestion, and hemorrhage.
- Irritability and Lethargy: Due to the discomfort and distress associated with the condition.
- Altered Mental Status: In severe cases, particularly when there is significant bowel compromise or shock.
Physical Examination
Abdomen: Often distended due to bowel obstruction, with tenderness upon palpation. An abdominal mass may be palpable, representing the intussuscepted bowel.
Rectal Exam: Reveals occult blood or frankly bloody stools, confirming the presence of gastrointestinal bleeding.
Investigations
Laboratory Tests
No Definitive Laboratory Test: Intussusception is primarily diagnosed based on clinical presentation and imaging findings. Laboratory tests may be performed to assess for dehydration, electrolyte imbalances, or secondary complications but do not reliably confirm or exclude the diagnosis.
Diagnostic Imaging
- Plain Abdominal Films: May reveal signs of bowel obstruction such as dilated loops of bowel and air-fluid levels but are not diagnostic of intussusception.
- Ultrasound: The preferred initial imaging modality, demonstrating the classic "target" sign or "pseudokidney" sign, indicative of the intussuscepted bowel within the intussuscipiens. Doppler flow can assess for signs of bowel ischemia.
- Barium/Air Enema: Both diagnostic and therapeutic, with the ability to visualize the intussusception and potentially reduce it through hydrostatic pressure or pneumatic pressure.
Management of Intussusception
Main Focus: Emergent Reduction of Obstructed Bowel
The primary goal in managing intussusception is the prompt reduction of the telescoped bowel to restore normal intestinal flow and prevent ischemia or perforation. Non-surgical reduction methods are often attempted initially, including:
Non-Surgical Reduction Techniques
- Barium Enema: Involves the administration of contrast material (barium sulfate) through the rectum under fluoroscopic guidance. The pressure exerted by the contrast material can often disengage the intussusception and restore normal bowel anatomy.
- Saline Enema: Similar to a barium enema but using saline solution instead of contrast material. It works by hydrostatic pressure to push the intussusception back into its normal position.
- Air Enema: Involves insufflating air into the bowel through the rectum, creating pressure to reduce the intussusception. This method has several advantages over barium enema.
Advantages of Air Enema over Barium Enema
- Easy to Administer: Air enema is simpler and quicker to perform compared to barium enema, requiring less preparation and setup time.
- Higher Success Rate: Studies have shown that air enema has a higher success rate in reducing intussusception compared to barium enema, making it a preferred initial option for non-surgical reduction.
- Less Radiation Exposure: Air enema involves minimal or no radiation exposure, making it safer for the pediatric population, particularly when repeated attempts at reduction are needed.
- Less Dangerous if Perforation Occurs: In the event of a bowel perforation during the procedure, air is less likely to cause peritoneal contamination or chemical peritonitis compared to barium, which can lead to a potentially serious chemical peritonitis if leaked into the peritoneal cavity.
Pathophysiology
- Failure of Normal Neural Crest Cell Migration: Hirschsprung disease (HD) results from the failure of neural crest cells to migrate properly along the gastrointestinal tract during embryonic development.
- Absent Ganglia in Myenteric and Submucosal Plexus: This leads to the absence of ganglion cells in the myenteric and submucosal plexuses, primarily in the distal rectum, and extending proximally.
Clinical Features
- Delayed Passage of Meconium: In 99% of full-term infants, meconium is typically passed within the first 48 hours of birth. Failure to do so is a hallmark sign of HD.
- Symptoms of Distal Bowel Obstruction: Clinical presentation mimics distal bowel obstruction and may include:
- Bilious or Feculent Emesis
- Abdominal Distension
- Failure to Pass Stool, especially within the first 48 hours of life.
- Explosive Passage of Stool after Rectal Examination (Blast Sign).
Diagnostic Work-up
- Contrast Enema: Typically reveals a contracted rectum with dilated bowel proximal to the affected area. Failure to evacuate contrast material within 24 hours can be diagnostic.
- Rectal Biopsy: The gold standard for diagnosis, revealing the absence of ganglion cells in affected segments.
Initial Management
- Resuscitation: Stabilization of the patient with intravenous fluids and electrolyte correction if needed.
- Colonic Washout: In some cases, a colonic washout may be performed to relieve obstruction.
- Colostomy: Temporary diversion of fecal flow may be necessary in severe cases, particularly if enterocolitis is present.
Definitive Treatment: Surgery
- Swenson Procedure: Proctolectomy with pull-through of normal ganglionated bowel to the anus.
- Duhamel Procedure: Posterior pull-through with side-to-side anastomosis to anganglionic rectum.
- Soave Procedure: Pulling ganglionated bowel through a sleeve of rectum.
- Transanal Pullthrough: Minimally invasive approach through the anus to remove the aganglionic segment.
Complications and Functional Outcome
- Enterocolitis: Risk of enterocolitis persists post-operatively and requires prompt recognition and treatment.
- Colostomy Related Complications: Stoma-related issues such as stenosis, prolapse, or skin irritation may occur.
- Chronic Constipation: Some patients may experience persistent constipation post-operatively.
- Fecal Continence: Achieving fecal continence may be challenging and may require bowel management programs or surgical revision.
- Urinary Continence: In some cases, urinary continence may be affected due to pelvic floor dysfunction or surgical complications.
- Anastomotic Leak/Stricture: Risk of anastomotic complications such as leaks or strictures exists post-operatively, requiring close monitoring and potential intervention.
Anorectal malformations (ARMs) are congenital anomalies where the anus and rectum do not develop properly. These defects occur in the lower end of the digestive tract and vary in severity, from mild forms with minor misplacement of the anus to complex anomalies involving other pelvic organs. The incidence of ARMs is approximately 1 in 5,000 live births, with a slight male predominance.
Pathophysiology
Anorectal malformations typically involve the anus being absent or abnormally positioned. In many cases, there is an associated fistulous tract that forms anteriorly, connecting the rectum to the urinary or genital tracts. This can result in the passage of fecal matter through the urinary or genital systems.
Clinical Features
ARMs are usually identified at birth by healthcare providers or parents. The clinical presentation includes:
- Absence of Anal Opening: The most immediate and obvious sign.
- Abnormally Positioned Anus: The anus may be located anteriorly to its normal position.
- Passage of Meconium: Fecal material may pass through the urine (in boys) or through the vagina (in girls), indicating a fistula.
- Meconium-Soiled Perineum: Meconium may be present on the skin of the perineum.
Delayed Presentation
In some cases, ARMs may present later with more severe symptoms:
- Inability to Pass Stool: Complete obstruction may occur if no fistulous tract is present.
- Abdominal Distension and Vomiting: Signs of bowel obstruction.
- Breathing Difficulties: Secondary to severe abdominal distension impacting diaphragmatic movement.
Management During the Neonatal Period
Immediate management aims to stabilize the neonate and prepare for definitive surgical correction. Initial steps include:
- IV Fluids: To maintain hydration.
- Nasogastric Tube (NGT): To decompress the stomach and prevent aspiration.
- IV Antibiotics: To prevent infection.
- Abdominal Ultrasound: To identify any associated urologic anomalies.
For boys, a gauze may be placed on the tip of the penis to check for the passage of meconium, indicating a fistula. If the patient does not present with significant abdominal distension, an X-ray is performed after 16-24 hours of observation to further evaluate the anatomy.
Operative Management
The type of surgical intervention depends on the specific anatomical details of the ARM.
-
Cutback Anoplasty
- Indication: Ectopic anus that is relatively close to the normal position.
- Procedure: Performed as soon as possible. An incision is made between the ectopic anus and the center of the sphincter, repositioning the anus.
-
Transposition Anoplasty
- Indication: Ectopic anus located at a larger distance from the normal position.
- Procedure: Similar to cutback anoplasty, but involves more extensive reconstruction of the perineal body to achieve proper positioning.
-
Posterior Sagittal Anorectoplasty (PSARP)
PSARP is indicated for more complex malformations and involves a sagittal incision through the perineum and sacrum to visualize and correct the anorectal anatomy precisely.
Complications
Despite corrective surgery, several complications can occur, impacting the child's long-term health:
- Fecal Incontinence: Due to insufficient sphincter function or nerve damage.
- Anal Stenosis: Narrowing of the anal opening leading to difficulty in passing stool.
- Fistula Recurrence: Reformation of the abnormal tract between the rectum and urinary or genital system.
- Wound Infection/Dehiscence: Breakdown of the surgical wound.
- Urinary Incontinence: Especially if there was significant involvement of the urinary tract.
- Vaginal Stenosis and Urethrovaginal Fistula: Specific complications in females, potentially impacting future reproductive and urinary function.
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Send your comments, corrections, explanations/clarifications and requests/suggestions