What You Will Learn
After reading this note, you should be able to...
- This content is not available yet.
Note Summary
This content is not available yet.
closeClick here to read a summary
Deafness:
- Refers to complete loss of hearing in the better ear, i.e., more than 90-100 dB.
- Or total loss of hearing.
Hearing Loss:
- Is a broad term defined as the impairment of hearing.
- Severity may vary from mild to profound.
- Profound HL = Deafness
- It is a significant social and educational handicap.
Based on:
- Type of Hearing Loss => Conductive Hearing Loss (CHL), Sensorineural Hearing Loss (SNHL), Mixed Hearing Loss (MHL)
- Site of Lesion: External Ear, Middle Ear, Inner Ear (Cochlear, Retrocochlea; Auditory Nerve, Central)
- Time of Onset: Congenital, Acquired
- Mode of Onset => Sudden or Insidious
- Rate of Progression => Rapid or Slow
- Degree => Mild, Moderate, Severe, Profound
- Laterality => Unilateral, Bilateral
- Aetiology => Infective, Metabolic, Noise Induced
| CRITERIA | SUBCATEGORY |
|---|---|
| Cause | Genetic (monogenic or multifactorial) Nongenetic |
| Association | Syndromic Nonsyndromic |
| Onset | Prelingual Postlingual |
| Type | Sensorineural Conductive Mixed |
| Severity | Mild (Loss of 21-40 dB) Moderate (Loss of 41-60 dB) Moderately severe (Loss of 61-80 dB) Severe (Loss of 81-100 dB) Profound (Loss of >100 dB) |
| Frequencies | Low (<500 Hz) Middle (501-2000 Hz) High (>2000 Hz) |
| *This classification is taken from Parving and Newton. | |
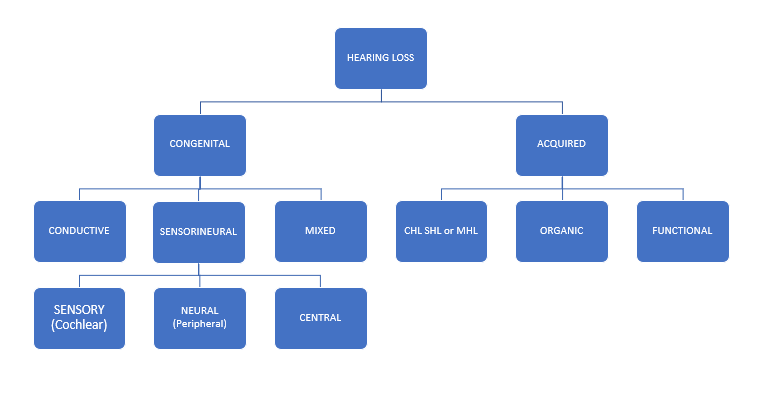
Conductive Hearing Loss
- Occurs when the sound conducting mechanism of the ear is defective.
- The pathology that interferes with the transmission of sound could be anywhere between the external auditory canal (EAC) to the footplate of the stapes.
- May be due to morphological changes in the middle and/or external ear.
Sensorineural Hearing Loss (SNHL)
- Occurs due to abnormality in the:
- cochlea,
- auditory nerve,
- neural pathway,
- or their central connection with the auditory cortex.
Mixed Hearing Loss
- Occurs when both conductive and sensorineural abnormalities are responsible for the hearing impairment.
| Grade of Impairment | Audiometric ISO value (average of 500, 1000, 2000, 4000 Hz) | Impairment description |
|---|---|---|
| 0 (no impairment) | 25 dB HL or less (better ear) | No or very slight hearing problems. Able to hear whispers |
| 1 (Slight impairment) | 26-40 dB HL (better ear) | Able to hear and repeat words spoken in normal voice at 1 metre |
| 2 (Moderate impairment) | 41-60 dB HL (better ear) | Able to hear and repeat words using raised voice at 1 metre |
| 3 (Severe impairment) | 61-80 dB HL (better ear) | Able to hear some words when shouted into better ear |
| 4 (Profound impairment deafness) | 81 dB HL or greater (better ear) | Unable to hear and understand even a shouted voice |
Acquired Causes of Conductive Hearing Loss (CHL)
External Canal
- Wax/Keratosis Obturans
- Foreign Body
- Trauma
- Otitis Externa
- Otomycosis
- Tumours, Osteoma, Exostosis
- Stenosis
- Fibrous Dysplasia, Wegener’s Granulomatosis
Middle Ear
- Acute/Chronic Otitis Media
- Barotrauma
- Perforated T.M (Tympanic Membrane)
- Otosclerosis
- Congenital Middle Ear Defect
- Trauma, Ossicular Disruption
- Stiffness or Hypermobility of the Ossicular Chain (Rheumatoid Arthritis)
- Tumours
Acquired Causes of Sensorineural Hearing Loss (SNHL)
Sensory
- Presbycusis
- Meniere’s Disease
- Noise Induced HL/Acoustic Trauma
- Ototoxicity
- Head Injury
- Mumps, Measles, Syphilis
- Vascular
- Ruptured Round Window Membrane
Neural
- Brain Tumours
- Demyelinating Diseases
- Trauma
- Presbycusis
- Acoustic Neuroma
- Viral Infection of Auditory Nerve
- Infection/Inflammation of Meninges
- Multiple Sclerosis
Other Acquired Causes of SNHL
- Trauma to the cochlea or retrocochlear, i.e., transverse fracture of the temporal bone
- Inflammatory: labyrinthitis - viral, bacterial, spirochaetal
- Noise: noise-induced hearing loss
- Metabolic: hyperthyroidism
- Familial: progressive sensorineural deafness
Congenital Causes of Conductive Hearing Loss (CHL)
Treacher Collins syndrome (mandibulo-facial dysostosis):
It is an autosomal dominant condition with complete penetrance and variable expression.
Features:
- Sloping palpebral fissures
- Fish mouth
- Malar hypoplasia
- Colobomas
- Microphthalmos
- Deformed pinna
- Absent external auditory canal (EAC)
- Facial nerve palsy
- Conductive Hearing Loss
Other Congenital Causes of Conductive Hearing Loss (CHL)
- Orofacial cranial syndrome
- Paget’s disease
- Ossicular anomalies: fixation, malformation, absence, discontinuity (fixation of stapes footplate, Fixation of malleus)
- Marfan’s syndrome
- Osteogenesis imperfecta
- Congenital cholesteatoma
- Meatal atresia
Congenital Causes of Sensorineural Hearing Loss (SNHL)
Non-Syndromic: Deafness Occurring Alone
- Scheibe’s syndrome (cochlear-saccular aplasia with normal bony labyrinth)
- Bing-Siebenmann syndrome (malformation of membranous labyrinth with osseous labyrinth)
- Alexander dysplasia: limited cochlea duct differentiation at the level of the basal coil (causes high-frequency SNHL).
- Large vestibular aqueduct syndrome: it is enlarged more than 1.5 mm on CT
Syndromic: Deafness Occurring with Other Anomalies
- Waardenburg's Syndrome (multi-colored eyes, white forelock, widest eyes, progressive HL)
- Usher's Syndrome (retinitis pigmentosa)
- Alport's Syndrome (deafness and kidney disease)
- Pendred's Syndrome (deafness and goiter)
Chromosomal Abnormalities
- Trisomy 13, 15
- Trisomy 21
Non-Genetic
- Intrauterine: TORCHS, DM, environmental hazards
- Perinatal: measles, herpes, chickenpox, HIV
- Neonatal: LBW (Low Birth Weight), Asphyxia, NNJ (Neonatal Jaundice), sepsis
- Developmental: delayed auditory maturation
- Hearing loss without any organic cause.
- Broadly includes the inability to hear because of psychological causes with no underlying lesion.
Classification: Conscious and Unconscious Origin
- Functional (Hysterical): More common among females. May be due to acute stress. The patient ceases to hear without being aware or in control of it; i.e., the deafness is subconscious, hysterical, psychosomatic.
- Malingering (Feigned Deafness): The malingerer listens but pretends not to hear. He is conscious but malingering/feigned.
Tests for Malingering
- General Tests: Examine the patient repeatedly and watch his/her behavior carefully. Tuning fork test and pure tone audiometry will not be consistent.
- Chimani Moos Test (Modified Weber Test): Place a tuning fork on the vertex; the patient confirms to hear only on the normal side. Then repeat the Weber test with the meatus blocked with a finger; he/she will deny hearing at all.
- Test During Sleep: Loud noise wakes a malingerer from sleep.
- Lambard’s Test (Reading and Noise Distraction Test)
- Stenger’s Test (Two Tuning Fork Test)
- Objective Tests: ABR (Auditory Brainstem Response), OAE (Otoacoustic Emissions), Acoustic Reflex Test
Treatment
- Psychotherapy:
- It is hearing loss caused by chronic exposure to noise of more than 85dB.
- Examples include industrial machineries, power drills, saws, engines, etc.
- It causes functional or structural changes in the cochlea.
- The effect depends on the frequency, intensity, duration, susceptibility, and pre-existing ear disease.
- Initially, the effect will be a Temporary Threshold Shift (TTS), from which hearing is reversible when the exposure stops, or
- Permanent Threshold Shift (PTS), which occurs later if the noise persists, causing irreversible damage (permanent deafness).
- Degenerative changes in the stria vascularis, hair cells, and supporting cells occur in chronic noise exposure.
- Noise induces vasospasm of the cochlear vessels and anoxia to the hair cells leading to damage.
- The 4KHz zone of the basilar membrane is in the basal turn of the cochlea and it is the first to be exposed to noise and the first to be affected.
Clinical Features
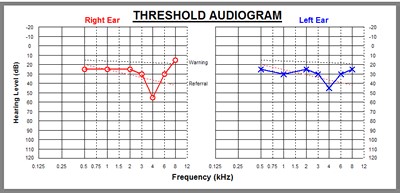
- Patient usually presents with tinnitus, hearing loss, and difficulty in comprehending speech.
- Pure tone audiometry will show a characteristic dip at 4KHz for both air and bone conduction.
Prevention
- Exposure to noise should not be more than 90dB for 8 hours per day, 5 working days per week.
- Use of ear protectors like ear plugs and muffs should be mandatory for workers in noisy factories.
- Public awareness and education against noise pollution.
- Pre-employment and periodic audiometric screening and ergonomics.
- It’s the capacity of a drug or chemical to damage the inner ear structure or derange its functions.
- It affects neurons of both cochlear and vestibular nerves.
- Drugs include aminoglycosides, cytotoxics, salicylates, quinine, diuretics, loop diuretics, macrolides (erythromycin).
- They present with tinnitus, hearing loss, and vertigo.
- Studies have shown that certain individuals may have a genetic predisposition or susceptibility to the ototoxic effect of certain drugs.
Clinical Features
- Tinnitus is usually the first symptom.
- Deafness and vertigo usually follow later.
- Poor renal function can accentuate ototoxicity to the drug.
Investigation
- Audiological test will show cochlear pattern of hearing loss.
Treatment
- Withdrawal of the offending drug.
- Hearing aids.
- It’s a sensorineural hearing loss which occurs due to the aging process. It is an auditory manifestation of senility. It increases with an increase in chronological age.
- Degenerative changes occur in the cells of the organ of Corti and nerve fibers.
- They present with a slow, progressive deafness, may be associated with tinnitus, vertigo, distortion of speech, recruitment may be positive.
- Agravating Factor: Smoking, alcoholism, coexisting illnesses (DM, HBP, hypothyroidism).
- Treatment: Psychological support, drugs, use of hearing aids.
Types:
- Conductive
- Sensorineural
- Idiopathic Sudden Sensorineural Hearing Loss (ISSNHL)
- Sudden Sensorineural Hearing Loss of Specific Cause
Sudden Conductive Hearing Loss
Causes:
- Traumatic perforation of tympanic membrane.
- Foreign body in the external auditory canal.
- Haemotympanum.
- Ossicular dyscontinuity.
- Aerotitis.
Treatment:
- Directed to the underlying cause.
Idiopathic Sudden Sensorineural Hearing Loss
It’s a deterioration of hearing involving:
- More than 30dB
- In at least 3 contiguous frequencies.
- Occurring within 3 days duration.
It is a diagnosis of exclusion, i.e., other specific causes should be ruled out.
Causes:
- Exact etiology is not known.
Prognosis:
2/3rd of patients recover fully within 2 weeks.
Sudden Sensorineural Hearing Loss of Specific Cause
It’s a deterioration of hearing involving more than 30dB in at least 3 adjacent frequencies, occurring within 3 days.
Specific Causes:
- May be due to vascular: vasospasm, thrombosis of inner ear end arteries.
- Oval window rupture.
- Viral infection: mumps, herpes zoster cochleitis.
- Other infections: Encephalitis, Syphilis.
- Trauma, perilymph fistula.
- Acoustic neuroma, immune complex, psychogenic, endolymphatic hydrops.
- Ototoxic drugs
- Multiple sclerosis
- Cogan’s disease
- Haematological: hyperviscosity syndromes, sickle cell disease
- Otitic Barotrauma
- Autoimmune Ag-Ab mediated destruction of Cochlea
Treatment
- Strict bed rest
- Steroid in tapering dosage, Tab prednisolone 1mg/kg
- Antiviral agents: Valcyclovir 1g tds for 5 days
- I.V. Low molecular weight dextran IV BD for 5 days
- I.V. histamine
- Vasodilator drugs (beta-histidine, nicotinic acid)
- O2, Carbogen (5% carbon dioxide and 95% oxygen) inhalation to increase perilymph oxygen tension.
- Transtympanic steroid injection may be of benefit
- Deaf mutism is the inability to acquire speech due to profound congenital or early acquired childhood sensorineural deafness in both ears.
- Profound or total deafness refers to hearing loss above 90dB.
- For normal speech, a child must hear sounds, imitates the words, and talks with time.
- The process is lost in deaf mute.
- It presents a special problem to ORL surgeon because of difficulties in detecting the deafness before the age of one.
- Causes can be congenital or acquired.
- Congenital can be genetic and non-genetic.
- Genetic involves conductive or sensorineural apparatus anomalies.
Neural Plasticity
- Ability of the CNS to be programmed to learn a task.
- Auditory plasticity and the ability to listen are lost by the age of 8 years.
- While the ability to develop good speech articulation occurs if speech sounds are heard by the age of 3 years.
Neural Plasticity and Childhood Deafness/Deaf Mutism
Classification:
- Prelingual: become deaf before acquiring speech
- Postlingual: speech acquired before becoming deaf.
- Perilingual: become deaf around the time of speech development
Management of Congenital Sensorineural Hearing Loss (SNHL)
- Normal hearing is necessary for the development of speech; hence, patients with severe HL fail to develop speech and thus remain deaf-mutes.
- Early detection and treatment are the goals.
- Refer patients to an ENT surgeon on time for comprehensive audiometry test and management.
Management of Congenital Sensorineural Hearing Loss (SNHL)
- In developed countries, routine hearing screening of the newborn is the common practice.
- This practice is not yet popular in developing countries.
- Parents are usually the first to suspect that the child is not hearing well.
- Such suspicion should not be ignored but be followed with comprehensive investigation.
Early Detection of Deafness
Investigate babies if there is parental suspicion due to:
- Failure to respond to sound properly.
- Failure to utter common words by 18 months to 2 years of age.
Babies at risk should be screened every 6 months
Risks:
- Babies born to consanguineous parents.
- Babies born to mothers with infection in early pregnancy, i.e., rubella, toxoplasmosis, German measles, herpes, syphilis.
- Use of ototoxic drugs in pregnancy.
- Perinatal complications like prematurity, anoxia, hemolytic disorders, low birth weight < 1.5kg.
- Perinatal viral infection, meningitis, jaundice.
Test of Hearing Acuity - Reflexes: Birth to 2 months
Reflexes:
- Startle reflex: Newborn responds to a loud sound by moving the head, legs, and arms.
- Cochleopalpebral (auriculo-palpebral) reflex: A loud noise made near a healthy infant causes the child to blink eyes (closure of palpebral fissure).
- Occulo gyric reflex: At 16 weeks, a loud sound produces horizontal movement of the eyeballs.
Test:
- Clap test: To test localization of sound; at 24 weeks, the child is able to localize sound.
Similarly, any sound made at 2-3 feet from the head of the baby: a baby with normal hearing will turn his head towards the sound source at the age of 7-9 months.
Other Hearing Tests:
- Free field audiometry: Hearing can be assessed by placing the child between two loud speakers in a soundproof room (after 6 months of age).
- Visual reinforcement audiometry: The child is conditioned to turn in the direction of sound, which is reinforced by light.
- Play audiometry: Child is conditioned or taught to play in response to the sound (children above 2-5 years).
- Pure tone audiometry: Above 5 years.
Objective Tests of Hearing
- Brain stem evoked response audiometry (BERA or ABR)
- Otoacoustic emission (OAE)
- Electrocochlography
- Impedance audiometry (tympanometry)
Deaf-mute - Evaluation
Age of Onset:
- At what age was deafness first suspected.
State of Development:
- What standard of education has the child reached?
- Any evidence of abnormal behavior or extreme introversion?
- What is the school report of the child’s intelligence and performance?
Treatment of Deaf Child
- Bilateral hearing aid
- Cochlear implantation
- Auditory training
- Language communication
Hearing Aids
Overview:
- It is an electro-acoustic device that amplifies sound to improve hearing.
- It assists the hearing-impaired individual to hear better.
- The signal processing system may be analog or digital.
Basic Components:
- A Microphone: Picks up sound from the environment and converts the sound to electrical energy.
- Amplifier: Amplifies the electrical sound energy to a louder volume.
- A Receiver: Converts the amplified electrical energy back to amplified sound waves and delivers it into the ear.
- A Power Source: Cell batteries.
Types of Hearing Aids - Ear Level Aids
Body Worn (BW): Worn at chest level, has the advantage of greater gain. Suitable for severe hearing loss.
Post Aural (BEHA - Behind the Ear): Has a stronger battery source and greater output. Suitable for moderate hearing loss.
In the Canal (ITC/ITE): Better cosmetic appeal, smaller output. Suitable for mild hearing loss.
Spectacle Hearing Aid: Fitted to the handle of eyeglasses.
Completely in the Canal Hearing Aid: Improved ITC.
Bone Anchored Hearing Aid: Has a bone vibrator (instead of a receiver) that fits over the mastoid to pass sound into the cochlea. Suitable for discharging ear or where there is canal atresia.
CROS Aids (Contralateral Routing of Signals): The microphone is placed in the poorer ear and routed to an earphone mounted behind the good ear.
Implantable Aids - Active Middle Ear Implants (MEI)
Overview:
- Uses the direct drive of the ossicular chain.
- Sound is converted into mechanical energy and directly transmitted to the ossicular chain, which vibrates in response to the converted sound signal.
- The device is coupled directly to the ossicle.
- It uses either a piezoelectric crystal (sensor) or electromagnetic mechanism.
Vibroplasty: The MEI is attached to the round window.
Suitable for:
- Moderate to severe cochlear hearing loss or SNHL.
- CHL with total loss of ossicles or failed tympanoplasties.
- MHL in cases of otosclerosis.
- Able to treat SNHL, CHL, and MHL.
Indications for Active Middle Ear Implants (MEI)
- Conductive hearing loss
- Mixed hearing loss
- Sensorineural hearing loss
- Failed medical treatment
- Refusal of surgical intervention
- Contraindicated surgery
Factors Influencing the Choice of Hearing Aid
Medical Factors:
- Type of hearing loss
- Site of lesion
- Other pathologies: Patency of the EAC, ear discharge, etc.
Non-Medical Factors:
- Cost
- Type
- Amplification character
- Ear mold
- General considerations
Cochlear Implant
Overview:
- It is an electrical device that emulates the transducer function of the cochlea, thereby stimulating the auditory nerve and restoring hearing.
- It bypasses the outer and middle ear.
- Causes electrical stimulation of the spiral ganglion.
Device Components:
External Component (placed behind the ear):
- Speech processor (with inbuilt-microphone)
- Radiofrequency coil with magnet
Internal Component:
- Receiver/stimulator package
- Active stimulating electrode
- Ground electrode
Cochlear Implant - Operation Process
- First, the sound is captured by a microphone.
- The microphone sends a signal to the speech processor.
- Sound signal is converted to electrical pulses by the speech processor.
- The radiofrequency link facilitates communication between the speech processor and the implant.
- The receiver/transmitter decodes the signal and presents it to the stimulation electrode within the cochlea.
- The sound energy is distributed to the cochlear in a frequency-specific manner along the basilar membrane.
Cochlear Implant - Indications
- Deafness due to cochlear pathology.
- (Central and auditory nerve causes are contraindications.)
- Bilateral severe to profound SNHL.
- Residual hearing with no speech understanding or speech development using a hearing aid.
- Prelingual deafness congenital or acquired before speech development.
- Postlingual deafness.
Auditory Brain Stem Implant - Indications
- Retrocochlear deafness: when the point of lesion is beyond the cochlea.
- Neurofibromatosis (NF2) patients with
Assistive Communication
- Speech/Lip Reading: Observing movement of lip and tongue.
- Auditory Training with Cue Speech: Lip reading plus hand signs.
- Finger Spelling
- Telecommunication Devices for the Deaf (TDD)
- Telephone Devices
- Computer Technology
Practice Questions
Check how well you grasp the concepts by answering the following questions...
- This content is not available yet.
Contributors
Jane Smith
She is not a real contributor.
John Doe
He is not a real contributor.
Send your comments, corrections, explanations/clarifications and requests/suggestions